17.4: Biological Basis of Schizophrenia Spectrum Disorder
- Page ID
- 140937
This page is a draft and under active development. Please forward any questions, comments, and/or feedback to the ASCCC OERI (oeri@asccc.org).
- Describe the principal features of schizophrenia spectrum disorders.
- Identify the difference between positive and negative symptoms in schizophrenia.
- Identify the biology thought to underlie the etiology of schizophrenia.
- Describe the dopamine hypothesis of schizophrenia.
Section Overview
Schizophrenia spectrum and other psychotic disorders are a category of psychological disorders encompassing an incredibly diverse range of characteristics, including distortions in perception, impairments in cognition, and abnormal motor activity. In addition, the symptoms vary greatly among individuals, as there are rarely two cases similar in presentation, course, or responsiveness to treatment (APA, 2013).
This category also includes schizophreniform disorder (a briefer version of schizophrenia), schizoaffective disorder (a mixture of psychosis and depression/mania symptoms), delusional disorder (the experience of only delusions), and brief psychotic disorder (psychotic symptoms that last only a few days or weeks). However, as many of the symptoms of these disorders overlap with schizophrenia, this disorder is the primary focus of this section.
Introduction to Schizophrenia
Originally termed dementia praecox (Latin for premature dementia), schizophrenia involves a diverse and complex set of symptoms, such as delusions, hallucinations, disorganized speech and behavior, abnormal motor behavior (including catatonia), anhedonia/amotivation and blunted affect/reduced speech (APA, 2013). Given this diversity of symptoms, and the fact that the presentation of symptoms can vary widely from case to case, it has been difficult for researchers and clinicians to precisely define schizophrenia as a disorder (Tandor, 2013). Growing evidence suggests that schizophrenia represents a broad and heterogenous syndrome, rather than a specific disorder, and is better classified along a psychosis spectrum (APA, 2013, Cuthbert & Morris, 2021).
When considering the symptoms of schizophrenia, it is common practice to divide the symptoms into positive symptoms (symptoms that demonstrate an excess of function) and negative symptoms (symptoms that represent a loss or reduction in function) (see Figure 17.4.2.1).
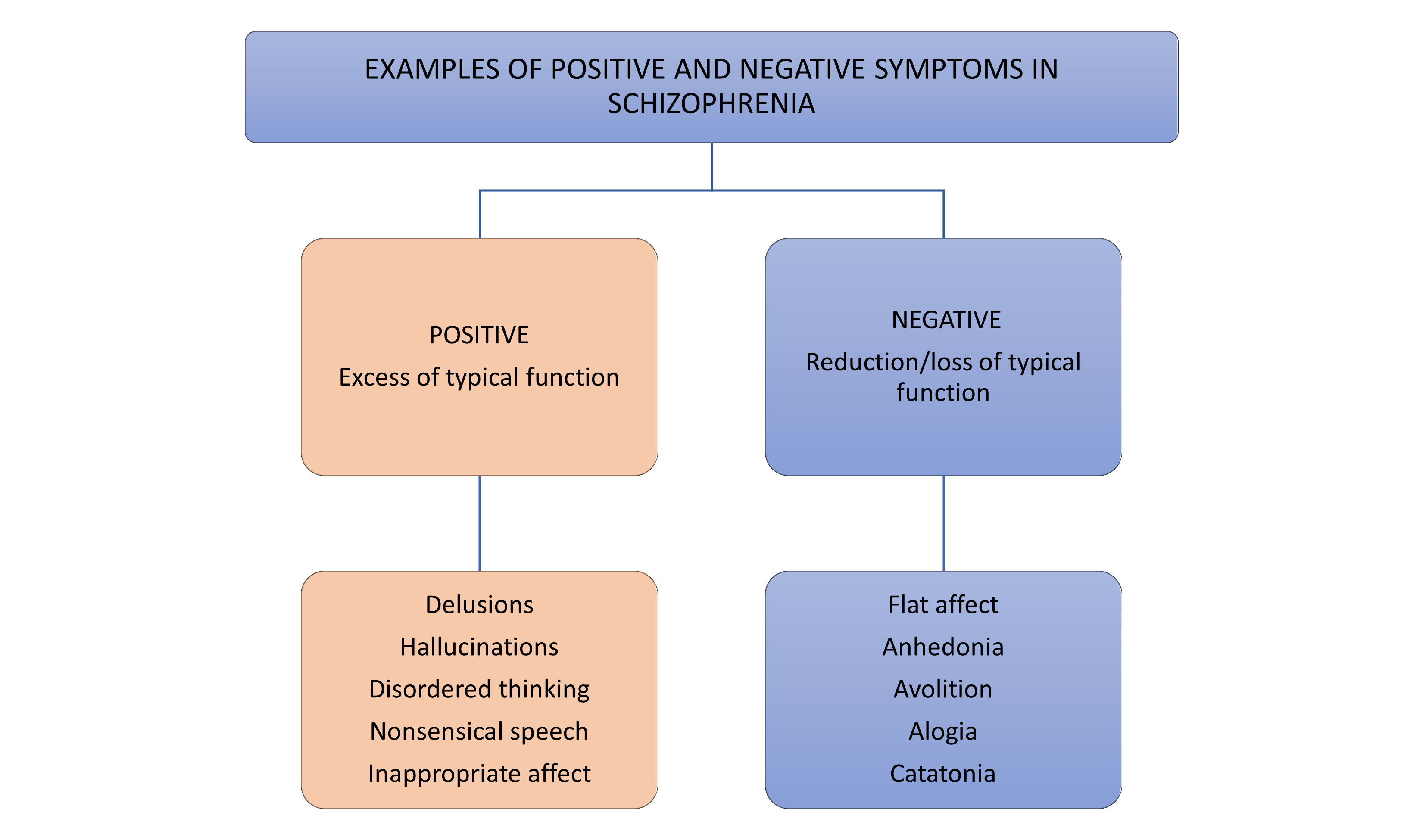
The most common positive symptoms are delusions and hallucinations. Delusions are “fixed beliefs that are not amenable to change in light of conflicting evidence” (APA, 2013, pp. 87). An individual suffering from delusions remains convinced in their belief, even when presented with clear, contradicting evidence. Researchers believe that delusions primarily relate to the social, emotional, educational, and cultural background of the individual (Arango & Carpenter, 2010). For example, an individual with schizophrenia who comes from a highly religious family is more likely to experience religious delusions (delusions of grandeur) than another type of delusion.
Hallucinations are perceptual experiences with no external stimulus (such as hearing voices when no one else is present). Hallucinations can occur in any sensory modality: auditory, visual, olfactory (smell), gustatory (taste), or somatic (touch), however the most common type are auditory hallucinations (APA, 2013). The content of these auditory hallucinations is frequently negative, making critical comments (“you’re worthless”) or telling the person what to do.
Negative symptoms typically involve an impairment in functions – cognitive, physical, and/or emotional. For example, anhedonia reflects a lack of apparent drive to engage in social or recreational activities. Importantly, this does not seem to reflect a lack of enjoyment in pleasurable activities or events (as is often seen in Depressive Disorders) (Llerena, et al., 2012) but rather a reduced drive or ability to take the steps necessary to obtain the potentially positive outcomes (Barch & Dowd, 2010). Flat affect and reduced speech (alogia) reflect a lack of showing emotions through facial expressions, gestures, and speech intonation, as well as a reduced amount of speech and increased pause frequency and duration.
Genetics and Epigenetics in Schizophrenia
Numerous family and twin studies have provided evidence that genetics play a significant role in an individual’s risk of developing schizophrenia (Henriksen, et al., 2017). However, as is the case with many psychological disorders, the genetics underlying schizophrenia have proven to be highly complex, heterogeneous, and polygenic. Furthermore, the wide variations in symptoms among cases (i.e., one individual may demonstrate only negative symptoms, while another may present only positive symptoms) makes it even more challenging to identify specific genes associated with risk for schizophrenia.
Genome-wide studies have identified more than 70 genes suspected of playing a role in producing schizophrenia (Flint & Munafò, 2014), and it is believed that the development of schizophrenia involves the cumulative effects of multiple genes, with most of these having only a small effect by themselves.
While our understanding of the genetic basis underlying schizophrenia is still developing, recent research has noted several genes associated with various aspects of brain development, including myelination and synaptic transmission (Smigielski, et al. 2020), that are also associated with an increased susceptibility to schizophrenia (Gürel, et al. 2020). It is now believed that this genetic susceptibility may be triggered by early environmental factors, through epigenetic mechanisms, and alter the course of neural development, leading to the later development of schizophrenia. (Gürel, et al. 2020.)
The Role of Neurotransmitters in Schizophrenia
Since the 1960s, it has been believed that many of the symptoms of schizophrenia were the result of an overactivity of dopamine. As with many of the psychological disorders, it is now understood that the biochemistry underlying schizophrenia is complex and involves multiple biological systems.
The Dopamine Hypothesis
Although the first antipsychotic drugs appeared in the 1950s, it was not well understood how these drugs were alleviating some of the symptoms of schizophrenia, nor why they also produced side effects, similar to those seen in patients with Parkinson’s disease (muscular rigidity, tremors, decrease in voluntary movement). It wasn’t until the late 1960s when further research made the notable discovery that the striatums of individuals with Parkinson’s disease were completely depleted of dopamine (Goetz, 2011). This discovery led researchers to further speculate that antipsychotic drugs might be producing their rigidity and tremor side effects by reducing dopamine activity, which then implied that many of the psychotic symptoms alleviated by these drugs were being caused by the overactivity of dopamine in the brain. These speculations developed into what eventually became known as the dopamine theory of schizophrenia (see Brisch, et al., 2014).
As researchers came to better understand the biological complexities of schizophrenia, the original version of the dopamine hypothesis no longer fit with our understanding of the disorder. This has led to the “revised dopamine hypothesis” (Brisch, et al., 2014). This revised hypothesis proposes that the increased dopamine transmission in the mesocorticolimbic areas (see Figure 17.4.2.2) and decreased dopamine transmission in the prefrontal cortex seen in individuals with schizophrenia account for many of their symptoms. (Pogarell, et al. 2012).
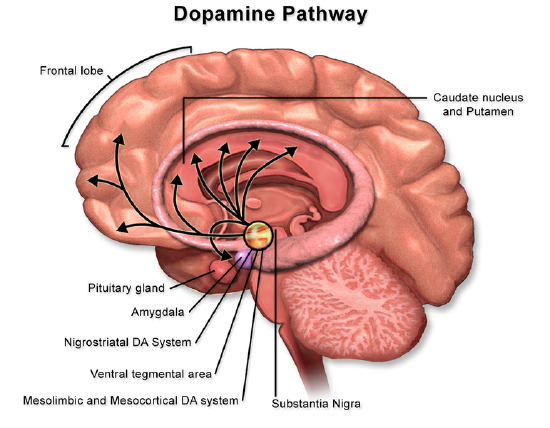
In addition to the mesolimbic brain areas, dopamine dysregulation has also been observed in the amygdala and prefrontal cortex, which are important for emotional processing, and differences in dopamine contents in the prefrontal cortex, cingulate cortex, and hippocampus between schizophrenia patients and healthy control subjects (Patel, et al., 2010). In particular, the dopamine system in the hippocampus is overactive in schizophrenia patients (Grace, 2012).
Neural Structures in Schizophrenia
There is a long and reliable history of research into the neural basis of schizophrenia. Neuroimaging studies have found a significant reduction in overall and specific brain region volumes, as well as tissue density of individuals with schizophrenia compared to healthy controls (Brugger & Howes, 2017). Additionally, there has been evidence of ventricle enlargement as well as volume reductions in the medial temporal lobe, which contains such structures as the amygdala (involved in emotion regulation), the hippocampus (involved in memory), as well as the neocortical surface of the temporal lobes (processing of auditory information) (Kurtz, 2015). Additional studies also indicate a reduction in the orbitofrontal regions of the brain, a part of the frontal lobe that is responsible for response inhibition (Kurtz, 2015).
.png?revision=1&size=bestfit&width=600&height=360)
References
Barch DM, Dowd EC. (2010). Goal representations and motivational drive in schizophrenia: the role of prefrontal-striatal interactions. Schizophr Bull., 36(5), 919-34. doi: 10.1093/schbul/sbq068.
Brisch, R., Saniotis, A., Wolf, R., Bielau, H., Bernstein, H. G., Steiner, J., Bogerts, B., Braun, K., Jankowski, Z., Kumaratilake, J., Henneberg, M., & Gos, T. (2014). The role of dopamine in schizophrenia from a neurobiological and evolutionary perspective: old fashioned, but still in vogue. Frontiers in psychiatry, 5, 47. https://doi.org/10.3389/fpsyt.2014.00047.
Brugger SP, Howes OD. (2017). Heterogeneity and Homogeneity of Regional Brain Structure in Schizophrenia: A Meta-analysis. JAMA Psychiatry. 74(11):1104-1111. doi:10.1001/jamapsychiatry.2017.2663. PMID: 28973084; PMCID: PMC5669456.
Cuthbert B.N. & Morris S.E. (2021). Evolving Concepts of the Schizophrenia Spectrum: A Research Domain Criteria Perspective. Frontiers in Psychiatry. 12. DOI=10.3389/fpsyt.2021.641319
Flint J, Munafò MR. (2014) Genetics: finding genes for schizophrenia. Curr Biol., 24(16), R755-7. doi: 10.1016/j.cub.2014.07.018.
Grace A. A. (2012). Dopamine system dysregulation by the hippocampus: implications for the pathophysiology and treatment of schizophrenia. Neuropharmacology, 62(3), 1342–1348. https://doi.org/10.1016/j.neuropharm.2011.05.011.
Gürel C, Kuşçu GC, Yavaşoğlu, A, Avcı, CB. (2020). The clues in solving the mystery of major psychosis: The epigenetic basis of schizophrenia and bipolar disorder. Neuroscience & Biobehavioral Reviews. 113. 51-61. https://doi.org/10.1016/j.neubiorev.2020.03.005.
Henriksen MG, Nordgaard J, Jansson LB. (2017). Genetics of Schizophrenia: Overview of Methods, Findings and Limitations. Frontiers in Human Neuroscience. 11. DOI=10.3389/fnhum.2017.00322
Kurtz MM, Trask CL, Rosengard R, Hyman S, Kremen L, Mehta S, Olfson R, Rispaud S, Zaidman S, Choi J. (2017). Verbal Learning and Memory Enhancement Strategies in Schizophrenia: A Randomized, Controlled Investigation. J Int Neuropsychol Soc. 23(4). 352-357. doi: 10.1017/S1355617717000042.
Llerena, K., Strauss, G. P., & Cohen, A. S. (2012). Looking at the other side of the coin: A meta-analysis of self-reported emotional arousal in people with schizophrenia. Schizophrenia Research, 142(1-3), 65–70. https://doi.org/10.1016/j.schres.2012.09.005.
Patel NH, Vyas NS, Puri BK, Nijran KS, Al-Nahhas A. (2010) Positron emission tomography in schizophrenia: a new perspective. J Nucl Med., 51(4). 511-20. doi: 10.2967/jnumed.109.066076.
Pogarell O, Koch W, Karch S, Dehning S, Müller N, Tatsch K, Poepperl G, Möller HJ. (2012). Dopaminergic neurotransmission in patients with schizophrenia in relation to positive and negative symptoms. Pharmacopsychiatry. 45(Suppl 1). 36-41. doi: 10.1055/s-0032-1306313.
Smigielski L, Jagannath V, Rössler W, Walitza S, Grünblatt E. (2020). Epigenetic mechanisms in schizophrenia and other psychotic disorders: a systematic review of empirical human findings. Mol Psychiatry. 25(8). 1718-1748. doi: 10.1038/s41380-019-0601-3. Epub 2020 Jan 6. PMID: 31907379.
Tandon R. (2013). Schizophrenia and other psychotic disorders in DSM-5. Clin Schizophr Relat Psychoses. 7(1), 16-9. doi: 10.3371/CSRP.TA.032513. PMID: 23538289.
Attributions
Chapter 17, Biological Basis of Psychological Disorders, 17.4. Biological Bases of Schizophrenia Spectrum and other psychotic disorders. Original material written by Amy E. Coren, PhD, Pasadena City College, is licensed under CC BY-NC-SA 4.0
. Text of section 17.4.5 adapted from Alexis Bridley & Lee W. Daffin Jr., Essentials of Abnormal Psychology, 6.1 Schizophrenia Spectrum and Other Psychotic Disorders by Washington State University licensed under CC-BY-NC-SA 4.0 International License. Retrieved from: https://opentext.wsu.edu/abnormalpsy...g-information/
Figure 17.4.1 CC BY-SA 4.0, Amy E. Coren, Ph.D. via original creation
Figure 17.4.2. CC BY-SA 4.0, BruceBlaus via Wikimedia Commons
Figure 17.4.3. CC BY-SA 4.0; BruceBlaus via Wikimedia Commons