3.2: Development of the Sexual Organs in the Embryo and Fetus
- Page ID
- 167175
Assigned females at birth are considered the “fundamental” sex—that is, without much chemical prompting, all fertilized eggs would develop into assigned females at birth. To be assigned male at birth, an individual must be exposed to the cascade of factors initiated by a single gene on the male Y chromosome. This is called the SRY (Sex-determining Region of the Y chromosome). Because females assigned at birth do not have a Y chromosome, they do not have the SRY gene. Without a functional SRY gene, an individual will be assigned female at birth.
In all embryos, the same group of cells has the potential to develop into the primordial sex specific gonads; this tissue is considered bipotential. The SRY gene actively recruits other genes that begin to develop the testes, and suppresses genes that are important in anatomical female development. As part of this SRY-prompted cascade, germ cells in the bipotential gonads differentiate into spermatogonia. Without SRY, different genes are expressed, oogonia form, and primordial follicles develop in the primitive ovary.
Soon after the formation of the testes, the Leydig cells begin to secrete testosterone. Testosterone can influence tissues that are bipotential to become male assigned at birth reproductive structures. For example, with exposure to testosterone, cells that could become either the glans penis or the glans clitoris form the glans penis. Without testosterone, these same cells differentiate into the clitoris.
Not all tissues in the reproductive tract are bipotential. The internal reproductive structures (for example the uterus, fallopian tubes, and part of the vagina in people assigned female at birth; and the epididymis, ductus deferens, and seminal vesicles in people assigned male at birth form from one of two rudimentary duct systems in the embryo.

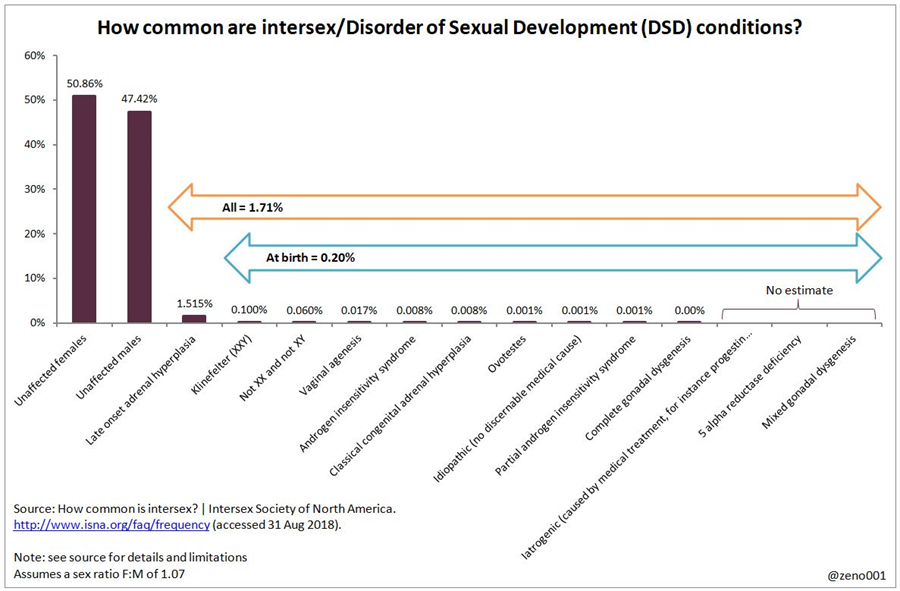
From a medical perspective, differentiated sex development or DSD can occur in approximately 1 in 100 individuals. The general term for people born with DSD is Intersex. This umbrella term is used for a range of variations that can occur when a person does not have the specific anatomy or chromosomal markers that would typically assign them either male or female. This is roughly the same statistical variation for green eyes or red hair factoring in a margin of error of 2%. According to our current understanding there are approximately twenty-five genes that have an impact on anatomical sex development. Taken together as an umbrella category, an estimated forty types of DSD have been medically recorded with approximately eight of those being the typical determinants of DSD across a normalized population sample.
As with most complex systems including biological organisms, simple models are often necessary to provide a shortcut to understanding. However, the risk in using these models is that they lack nuance and they rarely show the larger picture in context to other connected systems. Looping back to the spectra of medical sex, most secondary and primary school textbooks as well as some introductory level college texts use a simplified XX/XY model to demonstrate reproductive characteristics within a lifecycle. The XX/XY model is incomplete and lacks a large amount of understanding in how all the biological systems reflect and inform one another. Models and shortcuts are useful; for example, this work has used the term ‘assigned sex’ here to differentiate itself from sex as a larger psycho-social categorization but even that lacks nuance to a medical clinician since ‘assigned sex’ can be further broken down into chromosomal, gonadal or anatomical specialties as well as how hormones impact primary and secondary sex characteristics. These differentiations are particularly important in healthcare decisions as these specialties might be in completely different hospital departments.
The spectrum of difference in DSD and intersexed individuals can be visualized below:
As new data and training is filtered down slowly through the medical establishment, medical sex is now thought of to be closer to polygenetic traits since it results in a variety of expressions. Consider that it is not, nor has it ever been a strictly binary category.
This chapter focuses primarily on human anatomy but it is important to understand that as humans we are much more than our body parts. As we unpack the intersectionality of self throughout the course of this textbook we will come back to shed more light on the Intersex community. The link below is a good place to start. Intersex Community Q&A Series - YouTube
Further Sexual Development Occurs at Puberty
Puberty is the stage of development at which individuals become sexually mature. Though the outcomes of puberty significantly differ depending on assigned sex at birth, the hormonal control of the process is very similar. In addition, though the timing of these events varies between individuals, the sequence of changes that occur is fairly predictable for adolescents. As shown in Figure 27.18, a concerted release of hormones from the hypothalamus gonadotropin-releasing hormone (GnRH), the anterior pituitary-luteinizing hormone (LH) and follicle-stimulating hormone (FSH), and the gonads (either testosterone or estrogen) is responsible for the maturation of the reproductive systems and the development of secondary sex characteristics, which are physical changes that serve auxiliary roles in reproduction.
In addition to age, multiple factors can affect the age of onset of puberty, including genetics, environment, and psychological stress. One of the more important influences may be nutrition; historical data demonstrate the effect of better and more consistent nutrition on the age of menarche, (first menstruation) in the United States, which decreased from an average age of approximately 17 years of age in 1860 to the current age of approximately 12.75 years in 1960, as it remains today. Some studies indicate a link between puberty onset and the amount of stored fat in an individual. This effect is more pronounced in people assigned female at birth, but has also been documented in people assigned male at birth. Body fat, corresponding with secretion of the hormone leptin by adipose cells, appears to have a strong role in determining menarche. This may reflect to some extent the high metabolic costs of gestation and lactation.

Signs of Puberty
Different sex steroid hormone concentrations between the sexes also contribute to the development and function of secondary sexual characteristics. As assigned females at birth reach puberty, typically the first change that is visible is the development of the breast tissue. This is followed by the growth of axillary and pubic hair. A growth spurt normally starts at approximately age 9 to 11, and may last two years or more. During this time, their height can increase 3 inches a year. The next step in puberty is menarche, the start of menstruation.
For assigned males at birth, the growth of the testes is typically the first physical sign of the beginning of puberty, which is followed by growth and pigmentation of the scrotum and growth of the penis. The next step is the growth of hair, including armpit, pubic, chest, and facial hair. Testosterone stimulates the growth of the larynx and thickening and lengthening of the vocal folds, which causes the voice to drop in pitch. The first fertile ejaculations typically appear at approximately 15 years of age, but this age can vary widely. Unlike the early growth spurt observed in assigned females, assigned male’s growth spurts occur toward the end of puberty, at approximately age 16 to 18, and their height can increase as much as 4 inches a year. In some, pubertal development can continue through the early 20s.

A baby’s assigned sex is determined at conception, and the different genitalia of all fetuses develop from the same tissues in the embryo. View this animation to see a comparison of the development of structures of the different reproductive systems in a growing fetus. Where are the testes located for most of gestational time?
Review of Development of the Sexual Organs in the Embryo and Fetus
Human reproductive systems begin to develop soon after conception. A gene on the assigned male’s Y chromosome is called SRY. SRY is critical in stimulating a cascade of events that simultaneously stimulate testis development and repress the development of assigned female structures. Testosterone produced by Leydig cells in the embryonic testis stimulates the development of assigned male sexual organs. If testosterone is not present, female sexual organs will develop.
Whereas the gonads and some other reproductive tissues are considered bipotential, the tissue that forms the internal reproductive structures stems from ducts that will develop into only assigned male (Wolffian) or assigned female (Müllerian) structures. To be able to reproduce as an adult, one of these systems must develop properly and the other must degrade.
Further development of the reproductive systems occurs at puberty. The initiation of the changes that occur in puberty is the result of a decrease in sensitivity to negative feedback in the hypothalamus and pituitary gland, and an increase in sensitivity of the gonads to FSH and LH stimulation. These changes lead to increases in either estrogen or testosterone, in assigned female and male adolescents, respectively. The increase in sex steroid hormones leads to maturation of the gonads and other reproductive organs. The initiation of spermatogenesis begins in assigned males, and assigned females begin ovulating and menstruating. Increases in sex steroid hormones also lead to the development of secondary sex characteristics, such as breast development in assigned females and facial hair and larynx growth in assigned males.
The previous section highlights the ways in which fetal sexual anatomical formation occurs. It covers both the dymorphism associated with those assigned female at birth, those assigned male at birth and includes intersex anatomical formation which is varied in type. Human sexual reproduction involves the fertilization of an ovum by a sperm, the remaining portion of this chapter will be divided, in order to explore anatomical systems within bodies assigned female at birth and bodies assigned male at birth.


