10.5: Brain Mechanisms of Memory Disorders
- Page ID
- 139938
This page is a draft and under active development. Please forward any questions, comments, and/or feedback to the ASCCC OERI (oeri@asccc.org).
Learning Objectives
- Explain the roles of the hippocampus and medial temporal lobes in memory.
- Describe the case of H.M. and how it contributed to our understanding of the brain mechanisms in memory.
- Describe global amnesic syndrome.
- Discuss retrograde and anterograde amnesias including temporally graded amnesia.
- Describe amnesia of the frontal lobes.
- Discuss specific amnesias due to specific and circumscribed cortical damage.
Overview
We now examine the roles of the hippocampus and medial temporal lobes in memory and memory loss, focusing on amnesic syndromes associated with Korsakoff's Syndrome and Alzheimer's Disease. We also consider frontal lobe amnesia and highly specific forms of amnesia for highly specific types of information due to localized cortical damage. Damage to the amygdala disrupts emotional memories including memories of traumatic events. Diseases or other causes of cellular loss in the hippocampi can produce amnesia.
Amnesia, Hippocampus, and Medial Temporal Lobes
The Russian psychologist A. R. Luria (1968) has described the abilities of a man known as “S,” who seems to have unlimited memory. S remembers strings of hundreds of random letters for years at a time, and seems in fact to never forget anything. But what would this be like?
Shereshevsky, or “S,” the mnemonist studied by Luria was a man who almost never forgot. His memory appeared to be virtually limitless. He could memorize a table of 50 numbers in under 3 minutes and recall the numbers in rows, columns, or diagonals with ease. He could recall lists of words and passages that he had memorized over a decade before. Yet Shereshevsky found it difficult to function in his everyday life because he was constantly distracted by a flood of details and associations that sprung to mind. His case history suggests that remembering everything is not always a good thing. You may occasionally have trouble remembering where you parked your car, but imagine if every time you had to find your car, every single former parking space came to mind. The task would become impossibly difficult to sort through all of those irrelevant memories. Thus, forgetting is adaptive in that it makes us more efficient. The price of that efficiency is those moments when our memories seem to fail us (Schacter, 1999).
Clearly, remembering everything would be maladaptive, but what would it be like to remember nothing? We will now consider a profound form of forgetting called amnesia that is distinct from more ordinary forms of forgetting. Most of us have had exposure to the concept of amnesia through popular movies and television. Typically, in these fictionalized portrayals of amnesia, a character suffers some type of blow to the head and suddenly has no idea who they are and can no longer recognize their family or remember any events from their past. After some period of time (or another blow to the head), their memories come flooding back to them. Unfortunately, this portrayal of amnesia is not very accurate. What does amnesia typically look like?
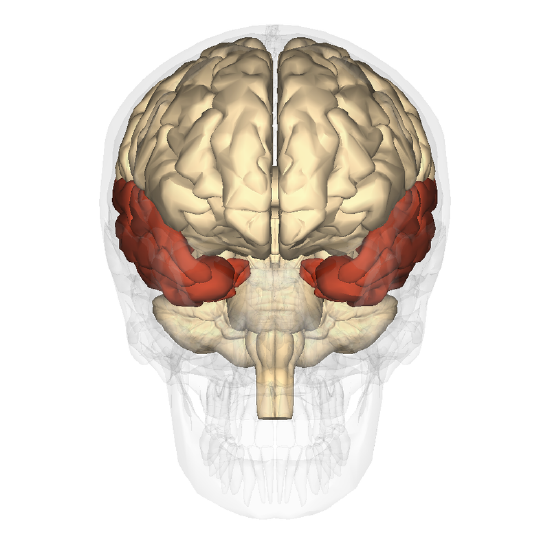
As previously discussed, the most widely studied amnesic patient was known by his initials H. M. (Scoville & Milner, 1957). H.M.'s disorder is an example of global amnesic syndrome characterized by severe anterograde amnesia and more moderate retrograde amnesia (see below). This syndrome results from bilateral lesions of the medial portion of the temporal lobe, and more specifically, of the hippocampus and its neighboring structures (the parahippocampal, entorhinal, and perirhinal cortices). These lesions can be due to surgical ablation, as in the case of H.M., or to other causes such as tumors, ischemic episodes, head traumas, and various forms of encephalitis.
As a teenager, H. M. suffered from severe epilepsy, and in 1953, he underwent surgery to have both of his medial temporal lobes removed to relieve his epileptic seizures. The medial temporal lobes encompass the hippocampus and surrounding cortical tissue. Although the surgery was successful in reducing H. M.’s seizures and his general intelligence was preserved, the surgery left H. M. with a profound and permanent memory deficit. From the time of his surgery until his death in 2008, H. M. was unable to learn new information, a memory impairment called anterograde amnesia. H. M. could not remember any event that occurred since his surgery, including highly significant ones, such as the death of his father. He could not remember a conversation he had a few minutes prior or recognize the face of someone who had visited him that same day. He could keep information in his short-term, or working, memory, but when his attention turned to something else, that information was lost for good. It is important to note that H. M.’s memory impairment was restricted to declarative memory, or conscious (explicit) memory for facts and events. H. M. could learn new motor skills and showed improvement on motor tasks even in the absence of any memory for having performed the task before (Corkin, 2002).
In addition to anterograde amnesia, H. M. also suffered from temporally graded retrograde amnesia. Retrograde amnesia refers to an inability to retrieve old memories that occurred before the onset of amnesia. Extensive retrograde amnesia in the absence of anterograde amnesia is very rare (Kopelman, 2000). More commonly, retrograde amnesia co-occurs with anterograde amnesia and shows a temporal gradient, in which memories closest in time to the onset of amnesia are lost, but more remote memories are retained (Hodges, 1994). In the case of H. M., he could remember events from his childhood, but he could not remember events that occurred a few years before the surgery.
Amnesiac patients with damage to the hippocampus and surrounding medial temporal lobes typically manifest a similar clinical profile as H. M. The degree of anterograde amnesia and retrograde amnesia depend on the extent of the medial temporal lobe damage, with greater damage associated with a more extensive impairment (Reed & Squire, 1998). Anterograde amnesia provides evidence for the role of the hippocampus in the formation of long-lasting declarative memories, as damage to the hippocampus results in an inability to create or consolidate this type of new long-term memory. Similarly, temporally graded retrograde amnesia can be seen as providing evidence for the importance of memory consolidation (Squire & Alvarez, 1995). A memory depends on the hippocampus until it is consolidated (or "fixed") and transferred into a more durable form that is stored in the cortex. According to this theory, an amnesiac patient like H. M. could remember events from his remote past because those memories were fully consolidated and no longer depended on the hippocampus, but instead had been transferred to other brain areas, primarily to particular areas of the cerebral cortex.
The classic amnesiac syndrome we have considered here is sometimes referred to as organic amnesia, and it is distinct from functional, or dissociative, amnesia. Functional amnesia involves a loss of memory that cannot be attributed to brain injury or any obvious brain disease and is typically classified as a mental disorder rather than a neurological disorder (Kihlstrom, 2005). The clinical profile of dissociative amnesia is very different from that of patients who suffer from amnesia due to brain damage or deterioration. Individuals who experience dissociative amnesia often have a history of trauma. Their amnesia is retrograde, encompassing autobiographical memories from a portion of their past. In an extreme version of this disorder, people enter a dissociative fugue state, in which they lose most or all of their autobiographical memories and their sense of personal identity. They may be found wandering in a new location, unaware of who they are and how they got there. Dissociative amnesia is controversial among research psychologists, as both the causes and existence of it have been called into question. The memory loss associated with dissociative amnesia is much less likely to be permanent than it is in organic amnesia.
Korsakoff's Amnesia
Another well-known form of amnesia is Korsakoff’s syndrome, encountered for the first time in chronic alcoholics. Korsakoff’s syndrome is similar to global amnesic syndrome, except that people with Korsakoff’s are more prone to confabulation to cover up gaps in their memories of their own past. Korsakoff’s syndrome is also known as diencephalic amnesia (or Wernicke-Korsakoff syndrome), because the vitamin B1 deficiency that results from alcoholism causes bilateral damage to the mammillary bodies of the hypothalamus. Similar symptoms are also produced by damage to the dorsomedial thalamic nuclei, the mammillothalamic tract, and the upper portion of the brainstem. Once again, other etiologies, such as strokes and tumors, can affect the same structures and produce the same results.
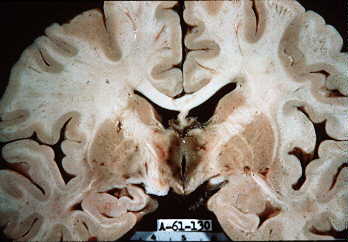
Figure \(\PageIndex{2}\): Brain affected by Wernicke-Korsakoff syndrome. Note the pigmentation of the grey matter around the third ventricle.
(Image Source: University of Texas (Houston); https://thebrain.mcgill.ca/flash/a/a...07_cr_oub.html; The Brain from Top to Bottom; Copyleft licence).
Alzheimer's Disease
In Alzheimer’s disease, beta-amyloid, an insoluble toxic substance, forms clumps known as “senile plaques” around the neurons. These plaques release free radicals that strip atoms from organic molecules that are vital to the neurons, including molecules in their cell membranes. Holes thus develop in these membranes, allowing large amounts of harmful substances to enter and kill the neurons. The memory circuits that depend on them, especially those in the hippocampus, are thus permanently damaged.
The National Institute on Aging reports on research indicating that the brains of Alzheimer's patients also contain neurofibrillary tangles which consist of a protein called tau. This protein normally plays a role in healthy microtubules inside neurons that assist with the transport of vital substances within the neuron cell body to the axon and dendrites. In Alzheimer's they form clumps that disrupt the neuron's transport system interfering with synaptic transmission. Complex interactions between beta-amyloid and tangles and other factors may then result in Alzheimer's. "It appears that abnormal tau accumulates in specific brain regions involved in memory. Beta-amyloid clumps into plaques between neurons. As the level of beta-amyloid reaches a tipping point, there is a rapid spread of tau throughout the brain" (https://www.nia.nih.gov/health/what-...eimers-disease; retrieved 5/11/2022).
Figure \(\PageIndex{3}\): Diagram showing changes of the brain caused by Alzheimer's disease. Note extreme shrinkage of cerebral cortex and hippocampus, and extensive deterioration and loss of brain tissue resulting in extremely enlarged cerebral ventricles (Image and caption from Wikimedia Commons; File:Alzheimer's disease brain comparison.jpg; https://commons.wikimedia.org/wiki/F...comparison.jpg; by SEVERESLICE_HIGH.JPG: ADEAR: "Alzheimer's Disease Education and Referral Center, a service of the National Institute on Aging," modifications by Garrondo; this work is in the public domain. This applies worldwide).
According to the National Institute on Aging, "at first, Alzheimer’s disease typically destroys neurons and their connections in parts of the brain involved in memory, including the entorhinal cortex and hippocampus. It later affects areas in the cerebral cortex responsible for language, reasoning, and social behavior. Eventually, many other areas of the brain are damaged. Over time, a person with Alzheimer’s gradually loses his or her ability to live and function independently. Ultimately, the disease is fatal" (https://www.nia.nih.gov/health/what-...eimers-disease; retrieved 5/11/2022).
Specific Cortical Damage and Memory Loss
There is also an amnesia of the frontal lobe due to damage at this site. People with this disorder do not suffer from global amnesia, but do show a memory deficit in tasks involving temporal planning of sequences of events. These people also have problems with the sources of newly acquired knowledge and have deficient meta-memory (they cannot make judgments about their memory’s contents).
Other types of damage to the cortex can cause forms of amnesia that are sometimes highly specific. For example, if the part of the cortex that perceives colors is damaged, people can lose their knowledge of color. And since the memory of colours is reconstructed at this same location, this memory disappears as well.
Other localized cortical lesions can prevent people from accessing certain items in their semantic memory and thus cause all sorts of specialized aphasias (language disorders).
Other Specific Forms of Memory Loss
A specific injury to the amygdala can prevent people from recording memories of traumatic events. In normal people, such memories are formed when particularly stressful conditions make certain details of a scene practically unforgettable.
Certain encephalopathies due to anoxias, ischemias, hypoglycemias, carbon monoxide poisoning, or prolonged epileptic attacks can cause the loss of large numbers of neurons in both hippocampi.
The pyramidal neurons of hippocampal area CA1, as well as the cortical neurons of layers 3, 5 and 6, the Purkinje cells, and the striate neurons are especially sensitive to lack of oxygen and energy.
Since these neurons are involved in various memory systems, malfunctions in their circuits inevitably lead to memory problems.
Thus, damage to the temporal lobes of the cortex can cause severe, permanent anterograde amnesia, as well as retrograde amnesia extending back from three to ten years before the accident.
When selective neuronal losses occur in area CA1 of the hippocampus, the resulting anterograde amnesia is just as severe, but the resulting retrograde amnesia generally remains slight (extending only one to two years before the accident).
Lastly, certain transitory global amnesias can be triggered suddenly, causing people to completely lose their memory for a few hours. Though these transitory amnesic episodes are frightening, they are brief and do not cause any permanent damage to the brain. They seem to be due to a temporary vascular insufficiency in the brain tissue.
Summary
Amnesiac patients show us what a life without memory would be like. Amnesiac patients suggest a special role for the hippocampus and surrounding medial temporal lobe structures in memory. Korsakoff's Syndrome is caused by vitamin B1 deficiency due to long term use of alcohol. Alzheimer's disease is associated with damage to neurons caused by plaques and tangles. Damage to specific cortical areas can cause very specific forms of memory loss including specific aphasias.
Outside Resources
(click resource for link)
- Web: Brain Case Study: Patient HM
- https://bigpictureeducation.com/brain-case-study-patient-hm
- Web: Self-experiment, Penny demo
- http://www.indiana.edu/~p1013447/dictionary/penny.htm
- Web: The Man Who Couldn’t Remember
- http://www.pbs.org/wgbh/nova/body/corkin-hm-memory.html
References
Corkin, S. (2002). What’s new with the amnesic patient H. M.? *Nature Reviews Neuroscience*, 3, 153–160.
Hodges, J. R. (1994). Retrograde amnesia. In A. Baddeley, B. A. Wilson, & F. Watts (Eds.), Handbook of Memory Disorders (pp. 81–107). New York: Wiley.
Kihlstrom, J. F. (2005). Dissociative disorders. Annual Review of Clinical Psychology, 1, 227– 253.
Kopelman, M. (2000). Focal retrograde amnesia and the attribution of causality: An exceptionally critical review. Cognitive Neuropsychology, 17, 585–621.
Luria, A. R. (1968). The mind of a mnemonist: A little book about a vast memory (L. Solataroff, Trans.). New York: Basic Books.
Reed, J. M. & Squire, L. R. (1998). Retrograde amnesia for facts and events: Findings from four new cases. Journal of Neuroscience, 18, 3943–3954.
Schacter, D. L. (1999). The seven sins of memory: Insights from psychology and cognitive neuroscience. American Psychologist, 54, 182–203.
Scoville, W. B. & Milner, B. (1957). Loss of recent memory after bilateral hippocampal lesions. Journal of Neurology, Neurosurgery, & Psychiatry, 20, 11–21.
Squire, L. R., & Alvarez, P. (1995). Retrograde amnesia and memory consolidation: A neurobiological perspective. Current Opinions in Neurobiology, 5, 169–177.
Attributions
Adapted by Kenneth A. Koenigshofer, PhD., from Forgetting and Amnesia by Nicole Dudukovic and Brice Kuhl, licensed by NOBA under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. Permissions beyond the scope of this license may be available in NOBA's Licensing Agreement. Dudukovic, N. & Kuhl, B. (2021). Forgetting and amnesia. In R. Biswas-Diener & E. Diener (Eds), Noba textbook series: Psychology. Champaign, IL: DEF publishers. Retrieved from http://noba.to/m38qbftg; Creative Commons License 


Korsakoff's Amnesia, Alzheimer's Disease, Specific Cortical Damage and Memory Loss, and Other Specific Forms of Memory Loss, adapted by Kenneth A. Koenigshofer, Ph.D., from "The Brain From Top to Bottom," Memory and the Brain; under Copyleft license.