8.6: Malnutrition
- Page ID
- 180242
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\dsum}{\displaystyle\sum\limits} \)
\( \newcommand{\dint}{\displaystyle\int\limits} \)
\( \newcommand{\dlim}{\displaystyle\lim\limits} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\(\newcommand{\longvect}{\overrightarrow}\)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\(\newcommand{\avec}{\mathbf a}\) \(\newcommand{\bvec}{\mathbf b}\) \(\newcommand{\cvec}{\mathbf c}\) \(\newcommand{\dvec}{\mathbf d}\) \(\newcommand{\dtil}{\widetilde{\mathbf d}}\) \(\newcommand{\evec}{\mathbf e}\) \(\newcommand{\fvec}{\mathbf f}\) \(\newcommand{\nvec}{\mathbf n}\) \(\newcommand{\pvec}{\mathbf p}\) \(\newcommand{\qvec}{\mathbf q}\) \(\newcommand{\svec}{\mathbf s}\) \(\newcommand{\tvec}{\mathbf t}\) \(\newcommand{\uvec}{\mathbf u}\) \(\newcommand{\vvec}{\mathbf v}\) \(\newcommand{\wvec}{\mathbf w}\) \(\newcommand{\xvec}{\mathbf x}\) \(\newcommand{\yvec}{\mathbf y}\) \(\newcommand{\zvec}{\mathbf z}\) \(\newcommand{\rvec}{\mathbf r}\) \(\newcommand{\mvec}{\mathbf m}\) \(\newcommand{\zerovec}{\mathbf 0}\) \(\newcommand{\onevec}{\mathbf 1}\) \(\newcommand{\real}{\mathbb R}\) \(\newcommand{\twovec}[2]{\left[\begin{array}{r}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\ctwovec}[2]{\left[\begin{array}{c}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\threevec}[3]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\cthreevec}[3]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\fourvec}[4]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\cfourvec}[4]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\fivevec}[5]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\cfivevec}[5]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\mattwo}[4]{\left[\begin{array}{rr}#1 \amp #2 \\ #3 \amp #4 \\ \end{array}\right]}\) \(\newcommand{\laspan}[1]{\text{Span}\{#1\}}\) \(\newcommand{\bcal}{\cal B}\) \(\newcommand{\ccal}{\cal C}\) \(\newcommand{\scal}{\cal S}\) \(\newcommand{\wcal}{\cal W}\) \(\newcommand{\ecal}{\cal E}\) \(\newcommand{\coords}[2]{\left\{#1\right\}_{#2}}\) \(\newcommand{\gray}[1]{\color{gray}{#1}}\) \(\newcommand{\lgray}[1]{\color{lightgray}{#1}}\) \(\newcommand{\rank}{\operatorname{rank}}\) \(\newcommand{\row}{\text{Row}}\) \(\newcommand{\col}{\text{Col}}\) \(\renewcommand{\row}{\text{Row}}\) \(\newcommand{\nul}{\text{Nul}}\) \(\newcommand{\var}{\text{Var}}\) \(\newcommand{\corr}{\text{corr}}\) \(\newcommand{\len}[1]{\left|#1\right|}\) \(\newcommand{\bbar}{\overline{\bvec}}\) \(\newcommand{\bhat}{\widehat{\bvec}}\) \(\newcommand{\bperp}{\bvec^\perp}\) \(\newcommand{\xhat}{\widehat{\xvec}}\) \(\newcommand{\vhat}{\widehat{\vvec}}\) \(\newcommand{\uhat}{\widehat{\uvec}}\) \(\newcommand{\what}{\widehat{\wvec}}\) \(\newcommand{\Sighat}{\widehat{\Sigma}}\) \(\newcommand{\lt}{<}\) \(\newcommand{\gt}{>}\) \(\newcommand{\amp}{&}\) \(\definecolor{fillinmathshade}{gray}{0.9}\)Many may not know that malnutrition is a problem that many children face, in both developing nations and the developed world. Even with the wealth of food in North America, many children grow up malnourished, or even hungry. The US Census Bureau characterizes households into the following groups:
- food secure
- food insecure without hunger
- food insecure with moderate hunger
- food insecure with severe hunger
Millions of children grow up in food-insecure households with inadequate diets due to both the amount of available food and the quality of food. In the United States, about 20 percent of households with children are food insecure to some degree. In half of those, only adults experience food insecurity, while in the other half both adults and children are considered to be food insecure, which means that children did not have access to adequate, nutritious meals at times.[1]
Growing up in a food-insecure household can lead to a number of problems. Deficiencies in iron, zinc, protein, and vitamin A can result in stunted growth, illness, and limited development. Federal programs, such as the National School Lunch Program, the School Breakfast Program, and Summer Feeding Programs, work to address the risk of hunger and malnutrition in school-aged children. They help to fill the gaps and provide children living in food-insecure households with greater access to nutritious meals.[2]
Internationally, World Health Organization (WHO, 2019) reported that 822 million people did not have sufficient food in 2018, and that this represented a rise of 11 million from the previous year. The largest number of undernourished people live in Asia. This affects child development in myriad ways, from being born low birth weight (20.5 million), to being affected by stunting under age 5 (149 million), and wasting under age 5 (almost 50 million).
There can be serious effects for children when there are deficiencies in their nutrition. Let’s explore a few types of nutritional concerns.
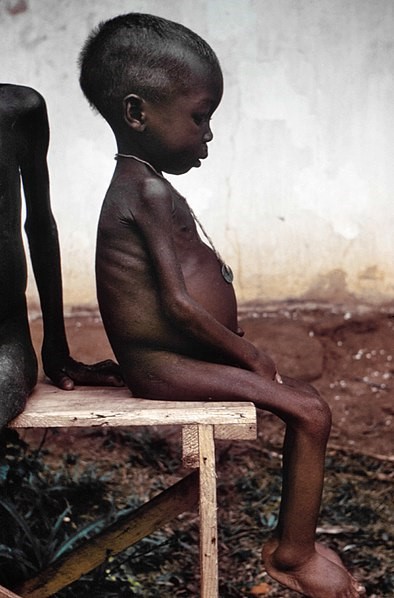
Wasting
Children in developing countries and countries experiencing the harsh conditions of war are at risk for two major types of malnutrition, also referred to as wasting. Infantile marasmus refers to starvation due to a lack of calories and protein. Children who do not receive adequate nutrition lose fat and muscle until their bodies can no longer function. Babies who are breastfed are much less at risk of malnutrition than those who are bottle-fed.
After weaning, children who have diets deficient in protein may experience kwashiorkor or the “disease of the displaced child,” often occurring after another child has been born and taken over breastfeeding. This results in a loss of appetite and swelling of the abdomen as the body begins to break down the vital organs as a source of protein.
Around the world the rates of wasting have been dropping. However, according to the World Health Organization and UNICEF, in 2018 there were 49.5 million children under the age of five that experienced these forms of wasting, (50 million in 2014 and 16 million were severely wasted according to UNICEF, 2015). Worldwide, these figures indicate that nearly one child in every 13 suffers from some form of wasting. The majority (about two third) of these children live in Asia, and almost all the rest in Africa. Wasting can occur as a result of severe food shortages, regional diets that lack certain proteins and vitamins, or infectious diseases that inhibit appetite (Latham, 1997).
The consequences of wasting depend on how late in the progression of the disease parents and guardians seek medical treatment for their children. Unfortunately, in some cultures families can not seek treatment early, and as a result by the time a child is hospitalized the child often dies within the first three days after admission (Latham, 1997). Several studies have reported long- term cognitive effects of early malnutrition (Galler & Ramsey, 1989; Galler, Ramsey, Salt & Archer, 1987; Richardson, 1980), even when home environments were controlled (Galler, Ramsey, Morley, Archer & Salt, 1990). Lower IQ scores (Galler et al., 1987), poor attention (Galler & Ramsey, 1989), and behavioral issues in the classroom (Galler et al., 1990) have been reported in children with a history of serious malnutrition in the first few years of life.[4]
Milk Anemia
About 9 million children in the United States are malnourished (Children’s Welfare, 1998). More still suffer from milk anemia, a condition in which milk consumption leads to a lack of iron in the diet. This can be due to the practice of giving toddlers milk as a pacifier-when resting, when riding, when waking, and so on. Appetite declines somewhat during toddlerhood and a small amount of milk (especially with added chocolate syrup) can easily satisfy a child’s appetite for many hours. The calcium in milk interferes with the absorption of iron in the diet as well.[5]
Failure to Thrive
Failure to thrive (FTT) occurs in children whose nutritional intake is insufficient for supporting normal growth and weight gain. FTT typically presents before two years of age, when growth rates are highest. Parents may express concern about picky eating habits, poor weight gain, or smaller size compared relative to peers of similar age. Physicians often identify FTT during routine office visits, when a child's growth parameters are not tracking appropriately on growth curves.
FTT can be caused by physical or mental issues within the child (such as errors of metabolism, acid reflux, anemia, diarrhea, Cystic fibrosis, Crohn’s disease, celiac disease, cleft palate, tongue tie, milk allergies, hyperthyroidism, congenital heart disease, etc.) It can also be caused by caregiver’s actions (environmental), including inability to produce enough breastmilk, inadequate food supply, providing an insufficient number of feedings, and neglect. These causes may also co-exist. For instance, a child who is not getting sufficient nutrition may act content so that caregivers do not offer feedings of sufficient frequency or volume, and a child with severe acid reflux who appears to be in pain while eating may make a caregiver hesitant to offer sufficient feedings.[6]
Attributions:
Child Growth and Development by Jennifer Paris, Antoinette Ricardo, and Dawn Rymond, 2019, is licensed under CC BY 4.0
[1]Coleman-Jensen A, et al. Household Food Security in the United States in 2010. US Department of Agriculture, Economic Research Report, no. ERR-125; 2011.
[2] Lifespan Development - Module 6: Middle Childhood by Lumen Learning references Psyc 200 Lifespan Psychology by Laura Overstreet, licensed under CC BY 4.0 (modified by Dawn Rymond)
Childhood University of Hawai’i at Mānoa Food Science and Human Nutrition Program by is licensed under CC BY-NC-SA 4.0 (modified by Dawn Rymond)
[3] Image by the CDC is in the public domain
[4] Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0
[5] Children’s Development by Ana R. Leon is licensed under CC BY 4.0
[6] Failure to Thrive by Wikipedia is licensed under CC BY-SA 3.0
World hunger is still not going down after three years and obesity is still growing – UN report, a press release in WHO

