12.2: Mood Disorders
- Last updated
- Save as PDF
- Page ID
- 12004
Stanford University, Washington University in St. Louis
Everyone feels down or euphoric from time to time, but this is different from having a mood disorder such as major depressive disorder or bipolar disorder. Mood disorders are extended periods of depressed, euphoric, or irritable moods that in combination with other symptoms cause the person significant distress and interfere with his or her daily life, often resulting in social and occupational difficulties. In this module, we describe major mood disorders, including their symptom presentations, general prevalence rates, and how and why the rates of these disorders tend to vary by age, gender, and race. In addition, biological and environmental risk factors that have been implicated in the development and course of mood disorders, such as heritability and stressful life events, are reviewed. Finally, we provide an overview of treatments for mood disorders, covering treatments with demonstrated effectiveness, as well as new treatment options showing promise.
learning objectives
- Describe the diagnostic criteria for mood disorders.
- Understand age, gender, and ethnic differences in prevalence rates of mood disorders.
- Identify common risk factors for mood disorders.
- Know effective treatments of mood disorders.
The actress Brooke Shields published a memoir titled Down Came the Rain: My Journey through Postpartum Depression in which she described her struggles with depression following the birth of her daughter. Despite the fact that about one in 20 women experience depression after the birth of a baby (American Psychiatric Association [APA], 2013), postpartum depression—recently renamed “perinatal depression”—continues to be veiled by stigma, owing in part to a widely held expectation that motherhood should be a time of great joy. In an opinion piece in the New York Times, Shields revealed that entering motherhood was a profoundly overwhelming experience for her. She vividly describes experiencing a sense of “doom” and “dread” in response to her newborn baby. Because motherhood is conventionally thought of as a joyous event and not associated with sadness and hopelessness, responding to a newborn baby in this way can be shocking to the new mother as well as those close to her. It may also involve a great deal of shame for the mother, making her reluctant to divulge her experience to others, including her doctors and family.

Feelings of shame are not unique to perinatal depression. Stigma applies to other types of depressive and bipolar disorders and contributes to people not always receiving the necessary support and treatment for these disorders. In fact, the World Health Organization ranks both major depressive disorder (MDD) and bipolar disorder (BD) among the top 10 leading causes of disability worldwide. Further, MDD and BD carry a high risk of suicide. It is estimated that 25%–50% of people diagnosed with BD will attempt suicide at least once in their lifetimes (Goodwin & Jamison, 2007).
What Are Mood Disorders?
Mood Episodes
Everyone experiences brief periods of sadness, irritability, or euphoria. This is different than having a mood disorder, such as MDD or BD, which are characterized by a constellation of symptoms that causes people significant distress or impairs their everyday functioning.
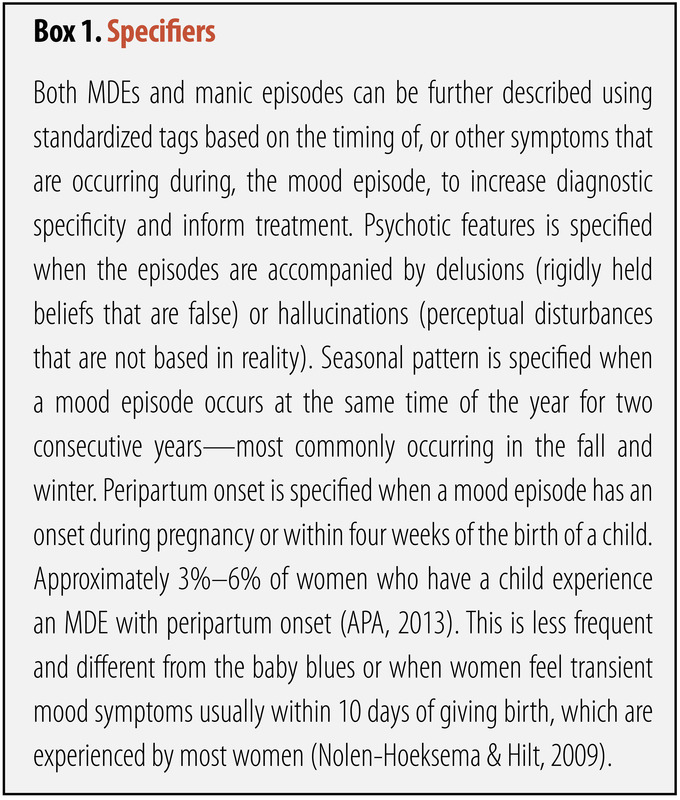
Major Depressive Episode
A major depressive episode (MDE) refers to symptoms that co-occur for at least two weeks and cause significant distress or impairment in functioning, such as interfering with work, school, or relationships. Core symptoms include feeling down or depressed or experiencing anhedonia—loss of interest or pleasure in things that one typically enjoys. According to the fifth edition of the Diagnostic and Statistical Manual (DSM-5; APA, 2013), the criteria for an MDE require five or more of the following nine symptoms, including one or both of the first two symptoms, for most of the day, nearly every day:
- depressed mood
- diminished interest or pleasure in almost all activities
- significant weight loss or gain or an increase or decrease in appetite
- insomnia or hypersomnia
- psychomotor agitation or retardation
- fatigue or loss of energy
- feeling worthless or excessive or inappropriate guilt
- diminished ability to concentrate or indecisiveness
- recurrent thoughts of death, suicidal ideation, or a suicide attempt
These symptoms cannot be caused by physiological effects of a substance or a general medical condition (e.g., hypothyroidism).
Manic or Hypomanic Episode
The core criterion for a manic or hypomanic episode is a distinct period of abnormally and persistently euphoric, expansive, or irritable mood and persistently increased goal-directed activity or energy. The mood disturbance must be present for one week or longer in mania (unless hospitalization is required) or four days or longer in hypomania. Concurrently, at least three of the following symptoms must be present in the context of euphoric mood (or at least four in the context of irritable mood):
- inflated self-esteem or grandiosity
- increased goal-directed activity or psychomotor agitation
- reduced need for sleep
- racing thoughts or flight of ideas
- distractibility
- increased talkativeness
- excessive involvement in risky behaviors
Manic episodes are distinguished from hypomanic episodes by their duration and associated impairment; whereas manic episodes must last one week and are defined by a significant impairment in functioning, hypomanic episodes are shorter and not necessarily accompanied by impairment in functioning.
Mood Disorders
Unipolar Mood Disorders
Two major types of unipolar disorders described by the DSM-5 (APA, 2013) are major depressive disorder and persistent depressive disorder (PDD; dysthymia). MDD is defined by one or more MDEs, but no history of manic or hypomanic episodes. Criteria for PDD are feeling depressed most of the day for more days than not, for at least two years. At least two of the following symptoms are also required to meet criteria for PDD:
- poor appetite or overeating
- insomnia or hypersomnia
- low energy or fatigue
- low self-esteem
- poor concentration or difficulty making decisions
- feelings of hopelessness
Like MDD, these symptoms need to cause significant distress or impairment and cannot be due to the effects of a substance or a general medical condition. To meet criteria for PDD, a person cannot be without symptoms for more than two months at a time. PDD has overlapping symptoms with MDD. If someone meets criteria for an MDE during a PDD episode, the person will receive diagnoses of PDD and MDD.
Bipolar Mood Disorders

Three major types of BDs are described by the DSM-5 (APA, 2013). Bipolar I Disorder (BD I), which was previously known as manic-depression, is characterized by a single (or recurrent) manic episode. A depressive episode is not necessary but commonly present for the diagnosis of BD I. Bipolar II Disorder is characterized by single (or recurrent) hypomanic episodes and depressive episodes. Another type of BD is cyclothymic disorder, characterized by numerous and alternating periods of hypomania and depression, lasting at least two years. To qualify for cyclothymic disorder, the periods of depression cannot meet full diagnostic criteria for an MDE; the person must experience symptoms at least half the time with no more than two consecutive symptom-free months; and the symptoms must cause significant distress or impairment.
It is important to note that the DSM-5 was published in 2013, and findings based on the updated manual will be forthcoming. Consequently, the research presented below was largely based on a similar, but not identical, conceptualization of mood disorders drawn from the DSM-IV (APA, 2000).
How Common Are Mood Disorders? Who Develops Mood Disorders?
Depressive Disorders
In a nationally representative sample, lifetime prevalence rate for MDD is 16.6% (Kessler, Berglund, Demler, Jin, Merikangas, & Walters, 2005). This means that nearly one in five Americans will meet the criteria for MDD during their lifetime. The 12-month prevalence—the proportion of people who meet criteria for a disorder during a 12-month period—for PDD is approximately 0.5% (APA, 2013).
Although the onset of MDD can occur at any time throughout the lifespan, the average age of onset is mid-20s, with the age of onset decreasing with people born more recently (APA, 2000). Prevalence of MDD among older adults is much lower than it is for younger cohorts (Kessler, Birnbaum, Bromet, Hwang, Sampson, & Shahly, 2010). The duration of MDEs varies widely. Recovery begins within three months for 40% of people with MDD and within 12 months for 80% (APA, 2013). MDD tends to be a recurrent disorder with about 40%–50% of those who experience one MDE experiencing a second MDE (Monroe & Harkness, 2011). An earlier age of onset predicts a worse course. About 5%–10% of people who experience an MDE will later experience a manic episode (APA, 2000), thus no longer meeting criteria for MDD but instead meeting them for BD I. Diagnoses of other disorders across the lifetime are common for people with MDD: 59% experience an anxiety disorder; 32% experience an impulse control disorder, and 24% experience a substance use disorder (Kessler, Merikangas, & Wang, 2007).
Women experience two to three times higher rates of MDD than do men (Nolen-Hoeksema & Hilt, 2009). This gender difference emerges during puberty (Conley & Rudolph, 2009). Before puberty, boys exhibit similar or higher prevalence rates of MDD than do girls (Twenge & Nolen-Hoeksema, 2002). MDD is inversely correlated with socioeconomic status (SES), a person’s economic and social position based on income, education, and occupation. Higher prevalence rates of MDD are associated with lower SES (Lorant, Deliege, Eaton, Robert, Philippot, & Ansseau, 2003), particularly for adults over 65 years old (Kessler et al., 2010). Independent of SES, results from a nationally representative sample found that European Americans had a higher prevalence rate of MDD than did African Americans and Hispanic Americans, whose rates were similar (Breslau, Aguilar-Gaxiola, Kendler, Su, Williams, & Kessler, 2006). The course of MDD for African Americans is often more severe and less often treated than it is for European Americans, however (Williams et al., 2007). Native Americans have a higher prevalence rate than do European Americans, African Americans, or Hispanic Americans (Hasin, Goodwin, Stinson & Grant, 2005). Depression is not limited to industrialized or western cultures; it is found in all countries that have been examined, although the symptom presentation as well as prevalence rates vary across cultures (Chentsova-Dutton & Tsai, 2009).
Bipolar Disorders
The lifetime prevalence rate of bipolar spectrum disorders in the general U.S. population is estimated at approximately 4.4%, with BD I constituting about 1% of this rate (Merikangas et al., 2007). Prevalence estimates, however, are highly dependent on the diagnostic procedures used (e.g., interviews vs. self-report) and whether or not sub-threshold forms of the disorder are included in the estimate. BD often co-occurs with other psychiatric disorders. Approximately 65% of people with BD meet diagnostic criteria for at least one additional psychiatric disorder, most commonly anxiety disorders and substance use disorders (McElroy et al., 2001). The co-occurrence of BD with other psychiatric disorders is associated with poorer illness course, including higher rates of suicidality (Leverich et al., 2003). A recent cross-national study sample of more than 60,000 adults from 11 countries, estimated the worldwide prevalence of BD at 2.4%, with BD I constituting 0.6% of this rate (Merikangas et al., 2011). In this study, the prevalence of BD varied somewhat by country. Whereas the United States had the highest lifetime prevalence (4.4%), India had the lowest (0.1%). Variation in prevalence rates was not necessarily related to SES, as in the case of Japan, a high-income country with a very low prevalence rate of BD (0.7%).

With regard to ethnicity, data from studies not confounded by SES or inaccuracies in diagnosis are limited, but available reports suggest rates of BD among European Americans are similar to those found among African Americans (Blazer et al., 1985) and Hispanic Americans (Breslau, Kendler, Su, Gaxiola-Aguilar, & Kessler, 2005). Another large community-based study found that although prevalence rates of mood disorders were similar across ethnic groups, Hispanic Americans and African Americans with a mood disorder were more likely to remain persistently ill than European Americans (Breslau et al., 2005). Compared with European Americans with BD, African Americans tend to be underdiagnosed for BD (and over-diagnosed for schizophrenia) (Kilbourne, Haas, Mulsant, Bauer, & Pincus, 2004; Minsky, Vega, Miskimen, Gara, & Escobar, 2003), and Hispanic Americans with BD have been shown to receive fewer psychiatric medication prescriptions and specialty treatment visits (Gonzalez et al., 2007). Misdiagnosis of BD can result in the underutilization of treatment or the utilization of inappropriate treatment, and thus profoundly impact the course of illness.
As with MDD, adolescence is known to be a significant risk period for BD; mood symptoms start by adolescence in roughly half of BD cases (Leverich et al., 2007; Perlis et al., 2004). Longitudinal studies show that those diagnosed with BD prior to adulthood experience a more pernicious course of illness relative to those with adult onset, including more episode recurrence, higher rates of suicidality, and profound social, occupational, and economic repercussions (e.g., Lewinsohn, Seeley, Buckley, & Klein, 2002). The prevalence of BD is substantially lower in older adults compared with younger adults (1% vs. 4%) (Merikangas et al., 2007).
What Are Some of the Factors Implicated in the Development and Course of Mood Disorders?
Mood disorders are complex disorders resulting from multiple factors. Causal explanations can be attempted at various levels, including biological and psychosocial levels. Below are several of the key factors that contribute to onset and course of mood disorders are highlighted.
Depressive Disorders
Research across family and twin studies has provided support that genetic factors are implicated in the development of MDD. Twin studies suggest that familial influence on MDD is mostly due to genetic effects and that individual-specific environmental effects (e.g., romantic relationships) play an important role, too. By contrast, the contribution of shared environmental effect by siblings is negligible (Sullivan, Neale & Kendler, 2000). The mode of inheritance is not fully understood although no single genetic variation has been found to increase the risk of MDD significantly. Instead, several genetic variants and environmental factors most likely contribute to the risk for MDD (Lohoff, 2010).

One environmental stressor that has received much support in relation to MDD is stressful life events. In particular, severe stressful life events—those that have long-term consequences and involve loss of a significant relationship (e.g., divorce) or economic stability (e.g., unemployment) are strongly related to depression (Brown & Harris, 1989; Monroe et al., 2009). Stressful life events are more likely to predict the first MDE than subsequent episodes (Lewinsohn, Allen, Seeley, & Gotlib, 1999). In contrast, minor events may play a larger role in subsequent episodes than the initial episodes (Monroe & Harkness, 2005).
Depression research has not been limited to examining reactivity to stressful life events. Much research, particularly brain imagining research using functional magnetic resonance imaging (fMRI), has centered on examining neural circuitry—the interconnections that allow multiple brain regions to perceive, generate, and encode information in concert. A meta-analysis of neuroimaging studies showed that when viewing negative stimuli (e.g., picture of an angry face, picture of a car accident), compared with healthy control participants, participants with MDD have greater activation in brain regions involved in stress response and reduced activation of brain regions involved in positively motivated behaviors (Hamilton, Etkin, Furman, Lemus, Johnson, & Gotlib, 2012).
Other environmental factors related to increased risk for MDD include experiencing early adversity (e.g., childhood abuse or neglect; Widom, DuMont, & Czaja, 2007), chronic stress (e.g., poverty) and interpersonal factors. For example, marital dissatisfaction predicts increases in depressive symptoms in both men and women. On the other hand, depressive symptoms also predict increases in marital dissatisfaction (Whisman & Uebelacker, 2009). Research has found that people with MDD generate some of their interpersonal stress (Hammen, 2005). People with MDD whose relatives or spouses can be described as critical and emotionally overinvolved have higher relapse rates than do those living with people who are less critical and emotionally overinvolved (Butzlaff & Hooley, 1998).
People’s attributional styles or their general ways of thinking, interpreting, and recalling information have also been examined in the etiology of MDD (Gotlib & Joormann, 2010). People with a pessimistic attributional style tend to make internal (versus external), global (versus specific), and stable (versus unstable) attributions to negative events, serving as a vulnerability to developing MDD. For example, someone who when he fails an exam thinks that it was his fault (internal), that he is stupid (global), and that he will always do poorly (stable) has a pessimistic attribution style. Several influential theories of depression incorporate attributional styles (Abramson, Metalsky, & Alloy, 1989; Abramson Seligman, & Teasdale, 1978).
Bipolar Disorders
Although there have been important advances in research on the etiology, course, and treatment of BD, there remains a need to understand the mechanisms that contribute to episode onset and relapse. There is compelling evidence for biological causes of BD, which is known to be highly heritable (McGuffin, Rijsdijk, Andrew, Sham, Katz, & Cardno, 2003). It may be argued that a high rate of heritability demonstrates that BD is fundamentally a biological phenomenon. However, there is much variability in the course of BD both within a person across time and across people (Johnson, 2005). The triggers that determine how and when this genetic vulnerability is expressed are not yet understood; however, there is evidence to suggest that psychosocial triggers may play an important role in BD risk (e.g., Johnson et al., 2008; Malkoff-Schwartz et al., 1998).
In addition to the genetic contribution, biological explanations of BD have also focused on brain function. Many of the studies using fMRI techniques to characterize BD have focused on the processing of emotional stimuli based on the idea that BD is fundamentally a disorder of emotion (APA, 2000). Findings show that regions of the brain thought to be involved in emotional processing and regulation are activated differently in people with BD relative to healthy controls (e.g., Altshuler et al., 2008; Hassel et al., 2008; Lennox, Jacob, Calder, Lupson, & Bullmore, 2004).
However, there is little consensus as to whether a particular brain region becomes more or less active in response to an emotional stimulus among people with BD compared with healthy controls. Mixed findings are in part due to samples consisting of participants who are at various phases of illness at the time of testing (manic, depressed, inter-episode). Sample sizes tend to be relatively small, making comparisons between subgroups difficult. Additionally, the use of a standardized stimulus (e.g., facial expression of anger) may not elicit a sufficiently strong response. Personally engaging stimuli, such as recalling a memory, may be more effective in inducing strong emotions (Isacowitz, Gershon, Allard, & Johnson, 2013).
Within the psychosocial level, research has focused on the environmental contributors to BD. A series of studies show that environmental stressors, particularly severe stressors (e.g., loss of a significant relationship), can adversely impact the course of BD. People with BD have substantially increased risk of relapse (Ellicott, Hammen, Gitlin, Brown, & Jamison, 1990) and suffer more depressive symptoms (Johnson, Winett, Meyer, Greenhouse, & Miller, 1999) following a severe life stressor. Interestingly, positive life events can also adversely impact the course of BD. People with BD suffer more manic symptoms after life events involving attainment of a desired goal (Johnson et al., 2008). Such findings suggest that people with BD may have a hypersensitivity to rewards.
Evidence from the life stress literature has also suggested that people with mood disorders may have a circadian vulnerability that renders them sensitive to stressors that disrupt their sleep or rhythms. According to social zeitgeber theory (Ehlers, Frank, & Kupfer, 1988; Frank et al., 1994), stressors that disrupt sleep, or that disrupt the daily routines that entrain the biological clock (e.g., meal times) can trigger episode relapse. Consistent with this theory, studies have shown that life events that involve a disruption in sleep and daily routines, such as overnight travel, can increase bipolar symptoms in people with BD (Malkoff-Schwartz et al., 1998).
What Are Some of the Well-Supported Treatments for Mood Disorders?
Depressive Disorders
There are many treatment options available for people with MDD. First, a number of antidepressant medications are available, all of which target one or more of the neurotransmitters implicated in depression.The earliest antidepressant medications were monoamine oxidase inhibitors (MAOIs). MAOIs inhibit monoamine oxidase, an enzyme involved in deactivating dopamine, norepinephrine, and serotonin. Although effective in treating depression, MAOIs can have serious side effects. Patients taking MAOIs may develop dangerously high blood pressure if they take certain drugs (e.g., antihistamines) or eat foods containing tyramine, an amino acid commonly found in foods such as aged cheeses, wine, and soy sauce. Tricyclics, the second-oldest class of antidepressant medications, block the reabsorption of norepinephrine, serotonin, or dopamine at synapses, resulting in their increased availability. Tricyclics are most effective for treating vegetative and somatic symptoms of depression. Like MAOIs, they have serious side effects, the most concerning of which is being cardiotoxic. Selective serotonin reuptake inhibitors (SSRIs; e.g., Fluoxetine) and serotonin and norepinephrine reuptake inhibitors (SNRIs; e.g., Duloxetine) are the most recently introduced antidepressant medications. SSRIs, the most commonly prescribed antidepressant medication, block the reabsorption of serotonin, whereas SNRIs block the reabsorption of serotonin and norepinephrine. SSRIs and SNRIs have fewer serious side effects than do MAOIs and tricyclics. In particular, they are less cardiotoxic, less lethal in overdose, and produce fewer cognitive impairments. They are not, however, without their own side effects, which include but are not limited to difficulty having orgasms, gastrointestinal issues, and insomnia.

Other biological treatments for people with depression include electroconvulsive therapy (ECT), transcranial magnetic stimulation (TMS), and deep brain stimulation. ECT involves inducing a seizure after a patient takes muscle relaxants and is under general anesthesia. ECT is viable treatment for patients with severe depression or who show resistance to antidepressants although the mechanisms through which it works remain unknown. A common side effect is confusion and memory loss, usually short-term (Schulze-Rauschenbach, Harms, Schlaepfer, Maier, Falkai, & Wagner, 2005). Repetitive TMS is a noninvasive technique administered while a patient is awake. Brief pulsating magnetic fields are delivered to the cortex, inducing electrical activity. TMS has fewer side effects than ECT (Schulze-Rauschenbach et al., 2005), and while outcome studies are mixed, there is evidence that TMS is a promising treatment for patients with MDD who have shown resistance to other treatments (Rosa et al., 2006). Most recently, deep brain stimulation is being examined as a treatment option for patients who did not respond to more traditional treatments like those already described. Deep brain stimulation involves implanting an electrode in the brain. The electrode is connected to an implanted neurostimulator, which electrically stimulates that particular brain region. Although there is some evidence of its effectiveness (Mayberg et al., 2005), additional research is needed.
Several psychosocial treatments have received strong empirical support, meaning that independent investigations have achieved similarly positive results—a high threshold for examining treatment outcomes. These treatments include but are not limited to behavior therapy, cognitive therapy, and interpersonal therapy. Behavior therapies focus on increasing the frequency and quality of experiences that are pleasant or help the patient achieve mastery. Cognitive therapies primarily focus on helping patients identify and change distorted automatic thoughts and assumptions (e.g., Beck, 1967). Cognitive-behavioral therapies are based on the rationale that thoughts, behaviors, and emotions affect and are affected by each other. Interpersonal Therapy for Depression focuses largely on improving interpersonal relationships by targeting problem areas, specifically unresolved grief, interpersonal role disputes, role transitions, and interpersonal deficits. Finally, there is also some support for the effectiveness of Short-Term Psychodynamic Therapy for Depression (Leichsenring, 2001). The short-term treatment focuses on a limited number of important issues, and the therapist tends to be more actively involved than in more traditional psychodynamic therapy.
Bipolar Disorders
Patients with BD are typically treated with pharmacotherapy. Antidepressants such as SSRIs and SNRIs are the primary choice of treatment for depression, whereas for BD, lithium is the first line treatment choice. This is because SSRIs and SNRIs have the potential to induce mania or hypomania in patients with BD. Lithium acts on several neurotransmitter systems in the brain through complex mechanisms, including reduction of excitatory (dopamine and glutamate) neurotransmission, and increasing of inhibitory (GABA) neurotransmission (Lenox & Hahn, 2000). Lithium has strong efficacy for the treatment of BD (Geddes, Burgess, Hawton, Jamison, & Goodwin, 2004). However, a number of side effects can make lithium treatment difficult for patients to tolerate. Side effects include impaired cognitive function (Wingo, Wingo, Harvey, & Baldessarini, 2009), as well as physical symptoms such as nausea, tremor, weight gain, and fatigue (Dunner, 2000). Some of these side effects can improve with continued use; however, medication noncompliance remains an ongoing concern in the treatment of patients with BD. Anticonvulsant medications (e.g., carbamazepine, valproate) are also commonly used to treat patients with BD, either alone or in conjunction with lithium.
There are several adjunctive treatment options for people with BD. Interpersonal and social rhythm therapy (IPSRT; Frank et al., 1994) is a psychosocial intervention focused on addressing the mechanism of action posited in social zeitgeber theory to predispose patients who have BD to relapse, namely sleep disruption. A growing body of literature provides support for the central role of sleep dysregulation in BD (Harvey, 2008). Consistent with this literature, IPSRT aims to increase rhythmicity of patients’ lives and encourage vigilance in maintaining a stable rhythm. The therapist and patient work to develop and maintain a healthy balance of activity and stimulation such that the patient does not become overly active (e.g., by taking on too many projects) or inactive (e.g., by avoiding social contact). The efficacy of IPSRT has been demonstrated in that patients who received this treatment show reduced risk of episode recurrence and are more likely to remain well (Frank et al., 2005).
Conclusion
Everyone feels down or euphoric from time to time. For some people, these feelings can last for long periods of time and can also co-occur with other symptoms that, in combination, interfere with their everyday lives. When people experience an MDE or a manic episode, they see the world differently. During an MDE, people often feel hopeless about the future, and may even experience suicidal thoughts. During a manic episode, people often behave in ways that are risky or place them in danger. They may spend money excessively or have unprotected sex, often expressing deep shame over these decisions after the episode. MDD and BD cause significant problems for people at school, at work, and in their relationships and affect people regardless of gender, age, nationality, race, religion, or sexual orientation. If you or someone you know is suffering from a mood disorder, it is important to seek help. Effective treatments are available and continually improving. If you have an interest in mood disorders, there are many ways to contribute to their understanding, prevention, and treatment, whether by engaging in research or clinical work.
Outside Resources
- Books: Recommended memoirs include A Memoir of Madness by William Styron (MDD); Noonday Demon: An Atlas of Depression by Andrew Solomon (MDD); and An Unquiet Mind: A Memoir of Moods and Madness by Kay Redfield (BD).
- Web: Visit the Association for Behavioral and Cognitive Therapies to find a list of the recommended therapists and evidence-based treatments.
- http://www.abct.org
- Web: Visit the Depression and Bipolar Support Alliance for educational information and social support options.
- http://www.dbsalliance.org/
Discussion Questions
- What factors might explain the large gender difference in the prevalence rates of MDD?
- Why might American ethnic minority groups experience more persistent BD than European Americans?
- Why might the age of onset for MDD be decreasing over time?
- Why might overnight travel constitute a potential risk for a person with BD?
- What are some reasons positive life events may precede the occurrence of manic episode?
Vocabulary
- Anhedonia
- Loss of interest or pleasure in activities one previously found enjoyable or rewarding.
- Attributional style
- The tendency by which a person infers the cause or meaning of behaviors or events.
- Chronic stress
- Discrete or related problematic events and conditions which persist over time and result in prolonged activation of the biological and/or psychological stress response (e.g., unemployment, ongoing health difficulties, marital discord).
- Early adversity
- Single or multiple acute or chronic stressful events, which may be biological or psychological in nature (e.g., poverty, abuse, childhood illness or injury), occurring during childhood and resulting in a biological and/or psychological stress response.
- Grandiosity
- Inflated self-esteem or an exaggerated sense of self-importance and self-worth (e.g., believing one has special powers or superior abilities).
- Hypersomnia
- Excessive daytime sleepiness, including difficulty staying awake or napping, or prolonged sleep episodes.
- Psychomotor agitation
- Increased motor activity associated with restlessness, including physical actions (e.g., fidgeting, pacing, feet tapping, handwringing).
- Psychomotor retardation
- A slowing of physical activities in which routine activities (e.g., eating, brushing teeth) are performed in an unusually slow manner.
- Social zeitgeber
- Zeitgeber is German for “time giver.” Social zeitgebers are environmental cues, such as meal times and interactions with other people, that entrain biological rhythms and thus sleep-wake cycle regularity.
- Socioeconomic status (SES)
- A person’s economic and social position based on income, education, and occupation.
- Suicidal ideation
- Recurring thoughts about suicide, including considering or planning for suicide, or preoccupation with suicide.
References
- Abramson, L. Y, Seligman, M. E. P., & Teasdale, J. (1978). Learned helplessness in humans: Critique and reformulation. Journal of Abnormal Psychology, 87, 49–74. doi: 10.1037/0021-843X.87.1.49
- Abramson, L. Y., Metalsky, G. I., & Alloy, L. B. (1989). Hopelessness depression: A theory-based subtype of depression. Psychological Review, 96, 358–373. doi: 10.1037/0022-3514.56.3.431
- Altshuler, L., Bookheimer, S., Townsend, J., Proenza, M. A., Sabb, F., Mintz, J., & Cohen, M. S. (2008). Regional brain changes in bipolar I depression: A functional magnetic resonance imaging study. Bipolar Disorders, 10, 708–717. doi: 10.1111/j.1399-5618.2008.00617.x
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author.
- Beck, A. T. (1967). Depression: Clinical, experimental, and theoretical aspects. New York, NY: Hoeber.
- Blazer, D., George, L. K., Landerman, R., Pennybacker, M., Melville, M. L., Woodbury, M., et al. (1985). Psychiatric disorders. A rural/urban comparison. Archives of General Psychiatry, 42, 651–656. PMID: 4015306. doi: 10.1001/archpsyc.1985.01790300013002
- Breslau, J., Aguilar-Gaxiola, S., Kendler, K. S., Su, M., Williams, D., & Kessler, R. C. (2006). Specifying race-ethnic differences in risk for psychiatric disorder in a US national sample. Psychological Medicine, 36, 57–68. doi: 10.1017/S0033291705006161
- Breslau, J., Kendler, K. S., Su, M., Gaxiola-Aguilar, S., & Kessler, R. C. (2005). Lifetime risk and persistence of psychiatric disorders across ethnic groups in the United States. Psychological Medicine, 35, 317–327. doi: 10.1017/S0033291704003514
- Brown, G. W., & Harris, T. O. (1989). Life events and illness. New York, NY: Guilford Press.
- Butzlaff, R. L., & Hooley, J. M. (1998). Expressed emotion and psychiatric relapse: A meta-analysis. Archives of General Psychiatry, 55, 547–552. doi: 10.1001/archpsyc.55.6.547
- Chentsova-Dutton, Y. E., & Tsai, J. L. (2009). Understanding depression across cultures. In I. H. Gotlib & C.L. Hammen (Eds.), Handbook of depression (2nd ed., pp. 363–385). New York, NY: Guilford Press.
- Conley, C. S., & Rudolph, K. D. (2009). The emerging sex difference in adolescent depression: Interacting contributions of puberty and peer stress. Development and Psychopathology, 21, 593–620. doi: 10.1017/S0954579409000327
- Dunner, D. L. (2000). Optimizing lithium treatment. Journal of Clinical Psychiatry, 61(S9), 76–81.
- Ehlers, C. L., Frank, E., & Kupfer, D. J. (1988). Social zeitgebers and biological rhythms: a unified approach to understanding the etiology of depression. Archives of General Psychiatry, 45, 948–952. doi: 10.1001/archpsyc.1988.01800340076012
- Ellicott, A., Hammen, C., Gitlin, M., Brown, G., & Jamison, K. (1990). Life events and the course of bipolar disorder. American Journal of Psychiatry, 147, 1194–1198.
- Frank, E., Kupfer, D. J., Ehlers, C. L., Monk, T., Cornes, C., Carter, S., et al. (1994). Interpersonal and social rhythm therapy for bipolar disorder: Integrating interpersonal and behavioral approaches. Behavior Therapy, 17, 143–149.
- Frank, E., Kupfer, D. J., Thase, M. E., Mallinger, A. G., Swartz, H. A., Fagiolini, A. M., et al. (2005). Two-year outcomes for interpersonal and social rhythm therapy in individuals with bipolar I disorder. Archives of General Psychiatry, 62, 996–1004. doi: 10.1001/archpsyc.62.9.996
- Geddes, J. R., Burgess, S., Hawton, K., Jamison, K., & Goodwin, G. M. (2004). Long-term lithium therapy for bipolar disorder: systematic review and meta-analysis of randomized controlled trials. American Journal of Psychiatry, 161, 217–222. doi: 10.1176/appi.ajp.161.2.217
- Gonzalez, J. M., Perlick, D. A., Miklowitz, D. J., Kaczynski, R., Hernandez, M., Rosenheck, R. A., et al. (2007). Factors associated with stigma among caregivers of patients with bipolar disorder in the STEP-BD study. Psychiatric Services, 58, 41–48. doi: 10.1176/appi.ps.58.1.41
- Goodwin, F. K., & Jamison, K. R. (2007). Manic-depressive illness: Bipolar disorders and recurrent depression. New York, NY: Oxford University Press.
- Gotlib, I. H., & Joormann, J. (2010). Cognition and depression: Current status and future directions. Annual Review of Clinical Psychology, 6, 285–312. doi: 10.1146/annurev.clinpsy.121208.131305
- Hamilton, J. P., Etkin, A., Furman, D. F., Lemus, M. G., Johnson, R. F., & Gotlib, I. H. (2012). Functional neuroimaging of major depressive disorder: A meta-analysis and new integration of baseline activation and neural response data. American Journal of Psychiatry, 169, 693–703.
- Hammen, C. (2005). Stress and depression. Annual Review of Clinical Psychology, 1, 293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938
- Harvey, A. G. (2008). Sleep and Circadian Rhythms in Bipolar Disorder: Seeking synchrony, harmony and regulation. American Journal of Psychiatry, 165, 820–829. doi: 10.1176/appi.ajp.2008.08010098
- Hasin, D. S., Goodwin, R. D., Sintson, F. S., & Grant, B. F. (2005). Epidemiology of major depressive disorder: Results from the National Epidemiological Survey on Alcoholism and Related Conditions. Archives of General Psychiatry, 62, 1097–1106. doi: 10.1001/archpsyc.62.10.1097
- Hassel, S., Almeida, J. R., Kerr, N., Nau, S., Ladouceur, C. D., Fissell, K., et al. (2008). Elevated striatal and decreased dorsolateral prefrontal cortical activity in response to emotional stimuli in euthymic bipolar disorder: No associations with psychotropic medication load. Bipolar Disorders, 10, 916–927. doi: 10.1111/j.1399-5618.2008.00641.x
- Isaacowitz, D. M., Gershon, A., Allard, E. S., & Johnson, S. L. (2013). Emotion in aging and bipolar disorder: Similarities, differences and lessons for further research. Emotion Review, 5, 312–320. doi: 10.1177/1754073912472244
- Johnson, S. L. (2005). Mania and dysregulation in goal pursuit: A review. Clinical Psychology Review, 25, 241–262. doi: 10.1016/j.cpr.2004.11.002
- Johnson, S. L., Cueller, A. K., Ruggero, C., Winett-Perlman, C., Goodnick, P., White, R., et al. (2008). Life events as predictors of mania and depression in bipolar I disorder. Journal of Abnormal Psychology, 117, 268–277. doi: 10.1037/0021-843X.117.2.268
- Johnson, S. L., Winett, C. A., Meyer, B., Greenhouse, W. J., & Miller, I. (1999). Social support and the course of bipolar disorder. Journal of Abnormal Psychology, 108, 558–566. doi: 10.1037/0021-843X.108.4.558
- Kessler, R. C., Berglund, P., Demler, O., Jim, R., Merikangas, K. R., & Walters, E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62, 593–602. doi: 10.1001/archpsyc.62.6.593
- Kessler, R. C., Birnbaum, H., Bromet, E., Hwang, I., Sampson, N., & Shahly, V. (2010). Age differences in major depression: Results from the National Comorbidity Surveys Replication (NCS-R). Psychological Medicine, 40, 225–237. doi: 10.1017/S0033291709990213
- Kessler, R. C., Merikangas, K. R., & Wang, P. S. (2007). Prevalence, comorbidity, and service utilization for mood disorders in the United States at the beginning of the 21st century. Annual Review of Clinical Psychology, 3, 137–158. doi: 10.1146/annurev.clinpsy.3.022806.091444
- Kilbourne, A. M., Haas, G. L., Mulsant, B. H., Bauer, M. S., & Pincus, H. A. (2004) Concurrent psychiatric diagnoses by age and race among persons with bipolar disorder. Psychiatric Services, 55, 931–933. doi: 10.1176/appi.ps.55.8.931
- Leichsenring, F. (2001). Comparative effects of short-term psychodynamic psychotherapy and cognitive-behavioral therapy in depression: A meta-analytic approach. Clinical Psychology Review, 21, 401–419. doi: 10.1016/S0272-7358(99)00057-4
- Lennox, B. R., Jacob, R., Calder, A. J., Lupson, V., & Bullmore, E. T. (2004). Behavioural and neurocognitive responses to sad facial affect are attenuated in patients with mania. Psychological Medicine, 34, 795–802. doi: 10.1017/S0033291704002557
- Lenox, R. H., & Hahn C. G. (2000). Overview of the mechanism of action of lithium in the brain: fifty-year update. Journal of Clinical Psychiatry, 61 (S9), 5–15.
- Leverich, G. S., Altshuler, L. L., Frye, M. A., Suppes, T., Keck, P. E. Jr, McElroy, S. L., et al. (2003). Factors associated with suicide attempts in 648 patients with bipolar disorder in the Stanley Foundation Bipolar Network. Journal of Clinical Psychiatry, 64, 506–515. doi: 10.4088/JCP.v64n0503
- Leverich, G. S., Post, R. M., Keck, P. E. Jr, Altshuler, L. L., Frye, M. A., Kupka, R. W., et al. (2007). The poor prognosis of childhood-onset bipolar disorder. Journal of Pediatrics, 150, 485–490. PMID: 17452221. doi: 10.1016/j.jpeds.2006.10.070
- Lewinsohn, P. M., Allen, N. B., Seeley, J. R., & Gotlib, I. H. (1999). First onset versus recurrence of depression: differential processes of psychosocial risk. Journal of Abnormal Psychology, 108, 483–489. doi: 10.1037/0021-843X.108.3.483
- Lewinsohn, P. M., Seeley, J. R., Buckley, M. E., & Klein, D. N. (2002). Bipolar disorder in adolescence and young adulthood. Child & Adolescent Psychiatric Clinics of North America, 11, 461–475. doi: 10.1016/S1056-4993(02)00005-6
- Lohoff, F. W. (2010). Overview of genetics of major depressive disorder. Current Psychiatry Reports, 12, 539–546. doi: 10.1007/s11920-010-0150-6
- Lorant, V., Deliege, D., Eaton, W., Robert, A., Philippot, P., & Ansseau, A. (2003). Socioeconomic inequalities in depression: A meta-analysis. American Journal of Epidemiology, 157, 98–112. doi: 10.1093/aje/kwf182
- Malkoff-Schwartz, S., Frank, E., Anderson, B. P., Sherrill, J. T., Siegel, L., Patterson, D., et al. (1998). Stressful life events and social rhythm disruption in the onset of manic and depressive bipolar episodes: a preliminary investigation. Archives of General Psychiatry, 55, 702–707. doi: 10.1001/archpsyc.55.8.702
- Mayberg, H. S., Lozano, A. M., Voon, V., McNeely, H. E., Seminowixz, D., Hamani, C., Schwalb, J. M., & Kennedy, S. H. (2005). Deep brain stimulation for treatment-resistant depression. Neuron, 45, 651–660. doi: 10.1016/j.neuron.2005.02.014
- McElroy, S. L., Altshuler, L. L., Suppes, T., Keck, P. E. Jr, Frye, M. A., Denicoff, K. D., et al. (2001). Axis I psychiatric comorbidity and its relationship to historical illness variables in 288 patients with bipolar disorder. American Journal of Psychiatry, 158, 420–426. doi: 10.1176/appi.ajp.158.3.420
- McGuffin, P., Rijsdijk, F., Andrew, M., Sham, P., Katz, R., Cardno, A. (2003). The heritability of bipolar affective disorder and the genetic relationship to unipolar depression. Archives of General Psychiatry, 60, 497–502. doi: 10.1001/archpsyc.60.5.497
- Merikangas, K. R., Akiskal, H. S., Angst, J., Greenberg, P. E., Hirschfeld, R. M., Petukhova, M., et al. (2007). Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Archives of General Psychiatry, 64, 543–552. doi: 10.1001/archpsyc.64.5.543
- Merikangas, K. R., Jin, R., He, J. P., Kessler, R. C., Lee, S., Sampson, N. A., et al. (2011). Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Archives of General Psychiatry, 68, 241–251. doi: 10.1001/archgenpsychiatry.2011.12
- Minsky, S., Vega, W., Miskimen, T., Gara, M., & Escobar, J. (2003). Diagnostic patterns in Latino, African American, and European American psychiatric patients. Archives of General Psychiatry, 60, 637–644. doi: 10.1001/archpsyc.60.6.637
- Monroe, S. M., & Harkness, K. L. (2011). Recurrence in major depression: A conceptual analysis. Psychological Review, 118, 655–674. doi: 10.1037/a0025190
- Monroe, S. M., & Harkness, K. L. (2005). Life stress, the “Kindling” hypothesis, and the recurrence of depression: Considerations from a life stress perspective. Psychological Review, 112, 417–445. doi: 10.1037/0033-295X.112.2.417
- Monroe, S.M., Slavich, G.M., Georgiades, K. (2009). The social environment and life stress in depression. In Gotlib, I.H., Hammen, C.L (Eds.) Handbook of depression (2nd ed., pp. 340-360). New York, NY: Guilford Press.
- Nolen-Hoeksema, S., & Hilt, L. M. (2009). Gender differences in depression. In I. H. Gotlib & Hammen, C. L. (Eds.), Handbook of depression (2nd ed., pp. 386–404). New York, NY: Guilford Press.
- Perlis, R. H., Miyahara, S., Marangell, L. B., Wisniewski, S. R., Ostacher, M., DelBello, M. P., et al. (2004). Long-term implications of early onset in bipolar disorder: data from the first 1000 participants in the systematic treatment enhancement program for bipolar disorder (STEP-BD). Biological Psychiatry, 55, 875–881. PMID: 15110730. doi: 10.1016/j.pscychresns.2007.10.003
- Rosa, M. A., Gattaz, W. F., Pascual-Leone, A., Fregni, F., Rosa, M. O., Rumi, D. O., … Marcolin, M. A. (2006). Comparison of repetitive transcranial magnetic stimulation and electroconvulsive therapy in unipolar non-psychotic refractory depression: a randomized, single-blind study. International Journal of Neuropsychopharmacology, 9, 667–676. doi: 10.1017/S1461145706007127
- Schulze-Rauschenbach, S. C., Harms, U., Schlaepfer, T. E., Maier, W., Falkai, P., & Wagner, M. (2005). Distinctive neurocognitive effects of repetitive transcranial magnetic stimulation and electroconvulsive therapy in major depression. British Journal of Psychiatry, 186, 410–416. doi: 10.1192/bjp.186.5.410
- Shields, B. (2005). Down Came the Rain: My Journey Through Postpartum Depression. New York: Hyperion.
- Sullivan, P., Neale, M. C., & Kendler, K. S. (2000). Genetic epidemiology of major depression: Review and meta-analysis. American Journal of Psychiatry, 157, 1552–1562. doi: 10.1176/appi.ajp.157.10.1552
- Twenge, J. M., & Nolen-Hoeksema, S. (2002). Age, gender, race, SES, and birth cohort differences on the Children’s Depression Inventory: A meta-analysis. Journal of Abnormal Psychology, 111, 578–588. doi: 10.1037/0021-843X.111.4.578
- Whisman, M. A., & Uebelacker, L. A. (2009). Prospective associations between marital discord and depressive symptoms in middle-aged and older adults. Psychology and Aging, 24, 184–189. doi: 10.1037/a0014759
- Widom, C. S., DuMont, K., & Czaja, S. J. (2007). A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Archives of General Psychiatry, 64, 49–56. doi: 10.1001/archpsyc.64.1.49
- Williams, D. R., Gonzalez, H. M., Neighbors, H., Nesse, R., Abelson, J. M., Sweetman, J., & Jackson, J. S. (2007). Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: Results from the National Survey of American Life. Archives of General Psychiatry, 64, 305–315. doi: 10.1001/archpsyc.64.3.305
- Wingo, A. P., Wingo, T. S., Harvey, P. D., & Baldessarini, R. J. (2009). Effects of lithium on cognitive performance: a meta-analysis. Journal of Clinical Psychiatry, 70, 1588–1597. doi: 10.4088/JCP.08r04972


