10.5: Aphasia
- Page ID
- 114836
Aphasia, from Sarah Harmon
Video Script
In the previous section Catherine Anderson described a little bit about aphasia. But this is an area that I think deserves much more discussion, so I’m going to create a whole mini-lecture on this. It also is something that affects me personally; I do not have aphasia but my husband does. He suffered a stroke about eight years ago, and while he is as humanly recovered as possible, he's still showing effects of aphasia. Not all the time, but occasionally. This is not uncommon; as more and more people survive strokes or massive head traumas and severe concussions, there's more evidence for aphasia. I think it's one of those areas that most people do need to understand, at least at a basic level.
Just like with every other section of this chapter, the information I’m going to provide you is as up-to-date as we can get for our understanding of the brain. There is much more that we are learning; in fact, almost weekly, if not monthly, there's a new study on various types of aphasia and how to improve and treat aphasia. We'll see some of this here, but know that this is a constantly evolving area of neurolinguistics and neurology as a whole.
What is aphasia? Aphasia is an issue with speech or language; we do see aphasia also in deaf folks who use a primary sign language, so this affects both spoken and signed language users. We know that, as you read before, language processing is predominantly a left-brain activity, while lexicon are stored throughout the brain. Primarily, the processing is in the left side and that the Broca’s Area, which is here in the front part of the temporal lobe on the left hemisphere, that is where much of the syntax and sentence formation occurs. The morphology and function words tend to reside there, too. Wernicke’s Area, which is more or less behind it—but that's kind of nebulous—that is controlling of semantics and processing. There are pieces in the middle; Exner’s Area controls writing, and that is in the motor cortex; the Articulate Fasciculus connects Broca’s and Wernicke’s Area; the Angular Gyrus is where a lot of the visual processing is done, and it's more towards the occipital lobe. Therefore, if you have a lesion in Broca’s Area, you tend to suffer from Broca’s Aphasia; if you have a lesion in the Wernicke’s Area, it tends to be Wernicke’s Aphasia. The name of the aphasia is tied to the primary area that is being affected.
Let's talk about these different aphasias.
Expressive or non-fluent aphasia is one entire category, and this is when the patient knows what they want to say, but they're not able to get it out. There are various levels of this aphasia. The lowest level is something called an anomia, where the motor skills of the patient are fine, but occasionally the patient is never able to come up with certain terms. Anomia frequently is called jargon aphasia, but jargon aphasia also affects Wernicke’s Area, so we'll talk about that in a minute. If the patient has trouble getting out language regularly—everybody suffers a bit when they're tired, and they can't express yourself. But if this is a chronic issue, so when you have the phrases and words that you want to say, but you can't get them out—that feeling that it's like at the tip of your tongue and they just not coming out—that is called either motor aphasia or dysarthria. That is what my husband has. If you're talking to him normally, most of the time you won't know that he has anything wrong. But if he's in a lot of pain, if he's very frustrated or upset, or if he's tired, he can't get out what he wants to say. He has to circumnavigate; he has to pivot and trying to think of a different way to say it. Again, all of us suffer from that a little bit when we're tired, or when we're sick, but certainly not at a chronic level; this is chronic. One of the things that dysarthria patients suffer from is extra wordiness, because they can't get out exactly what they're trying to say. They have to pivot, frequently that results in the patient getting very wordy. Frequently, it feels like they're going on a tangent, to a different conversation, and that's not actually the case. They desperately want to stay in-lane, as it were; they just can't because they've had to find other ways to describe their thoughts. Motor aphasia or dysarthria is challenging, and most patients who have dysarthria or motor aphasia also have some kind of coordination issue. In my husband's case, he certainly has a balance issue, and he also has certain dexterity issues, that are related to a stroke. A more aggravated version would be Broca’s Aphasia. This aphasia can vary greatly, but by and large, if you have Broca’s Aphasia, you are not putting sentences together fluently; this is why we call it non-fluent aphasia. Everything comes out in chunks; it may not be the correct term at first, and/or you may have to pivot and think of something else you know. Importantly, you know that you're not communicating properly. Unfortunately, many Broca’s aphasics, if they cannot find any fluency, if they are permanently non-fluent, most of them just stop talking, or only talk to one or two very trusted folks. They're very aware that they are not able to communicate.
Below in 10.5.2, you have examples videos of a young lady named Sarah Scott. She is a British woman who, when she was 18 years old, suffered a massive stroke in her English class. As a result, she ended up with Broca’s Aphasia. On the YouTube channel that her mother created and now she's a heavy participant of she shows her progress over time. I want you to watch the videos, at least in part. When you see Sarah Scott one year after her stroke, she shows very hesitant speech; stuff just isn't coming out. She doesn't have the right word, or she might know the word but it just is blocked and she can't do it.
Broca’s aphasics, however, do improve, with many, to the point of just having dysarthria. Check out Sarah’s progress over the years—and this is just a couple of videos; there are many more on their channel. The same happened with my husband. When he first had his stroke, the first 2-3 months he was in Broca’s Aphasia-land; he was able to get out much of what he wanted to say, but there was great hesitation, frequently searching for the word and not quite getting there. Between therapy and genetics, and the fact that he was young—he was only 41 when he had a stroke—that helped him to recover, to the point of dysarthria. As I said, if he's having a good day, with good energy and in good mood, you would never know he ever had a stroke. On a bad day, you suspect something has happened.
When we talk about receptive aphasias, frequently called fluent aphasias, that's a different story. Wernicke’s Aphasia is the main one here, and this is when the patient’s language is a jumble, that what the person says has no semantics; they're completely gone. Sometimes in extreme cases that can be called jargon aphasia because you're saying that the person is not able to come up with the right terms; the syntax is frequently decent, if not intelligible. There's grammaticality in many cases, but the semantics is wrong, the compositionality is wrong, nothing to do with anything else. When the lesion is away from the Wernicke’s Area and closer to the Articulate Fasciculus—closer to Broca’s Area—we see conduction aphasia, which is when the person can hear and understand and perform but can't repeat. They otherwise speak normally, but if you say, “Could you repeat that back? Can you repeat back what I said?” they can't do it. It is interesting to know that while dyslexia as a whole is still being researched, and we still don't really know a lot about how and why it forms, there are types of acquired dyslexia that have to do with language, specifically reading. These acquired dyslexia conditions do involve Wernicke’s Area, so the person with acquire dyslexia frequently is able to speak perfectly fine, but because of where the lesion is, at the back part of Wernicke’s Area affecting reading and processing, they're not able to read and comprehend.
There is important to underscore with respect to aphasia. Aphasia is fairly permanent; it may progress to a state that is better, especially with expressive or non-fluent aphasias, but even with receptive aphasias you can see progress, where the patient does get back some of their linguistic facility. But it never goes away; it's never 100% healed, at least not at this point in time. Certainly, there are factors that are in the favor or against improvement. When a younger person under the age of 60 has some kind of trauma or lesion, the brain is able to adapt; the brain is able to reroute a lot quicker and especially if that person was otherwise decently healthy. Even though a patient is not able to fully recover from any aphasia, there can be progress. As I mentioned earlier, there tends to be more progress with expressive aphasics. However, Wernicke’s patients, in particular, are a different story; they very rarely recover. Although it can happen, it is very difficult. Conduction aphasia has much more success, and usually patients are able to recover some of that ability. It is something that takes a lot of time and there's a number of factors that need to be included.
Just to give you a written example of aphasic patients, specifically Broca’s Aphasia versus Wernicke’s Aphasia. You can see that with Broca’s Aphasia, there's a lot of pausing—that's what the ellipses represent—that more or less, you can understand what the person is trying to say. They were asked about a dental appointment and they described what happened. But notice how many times the patient has to pivot and start saying one thing in order to really say another thing. See the graphics below.
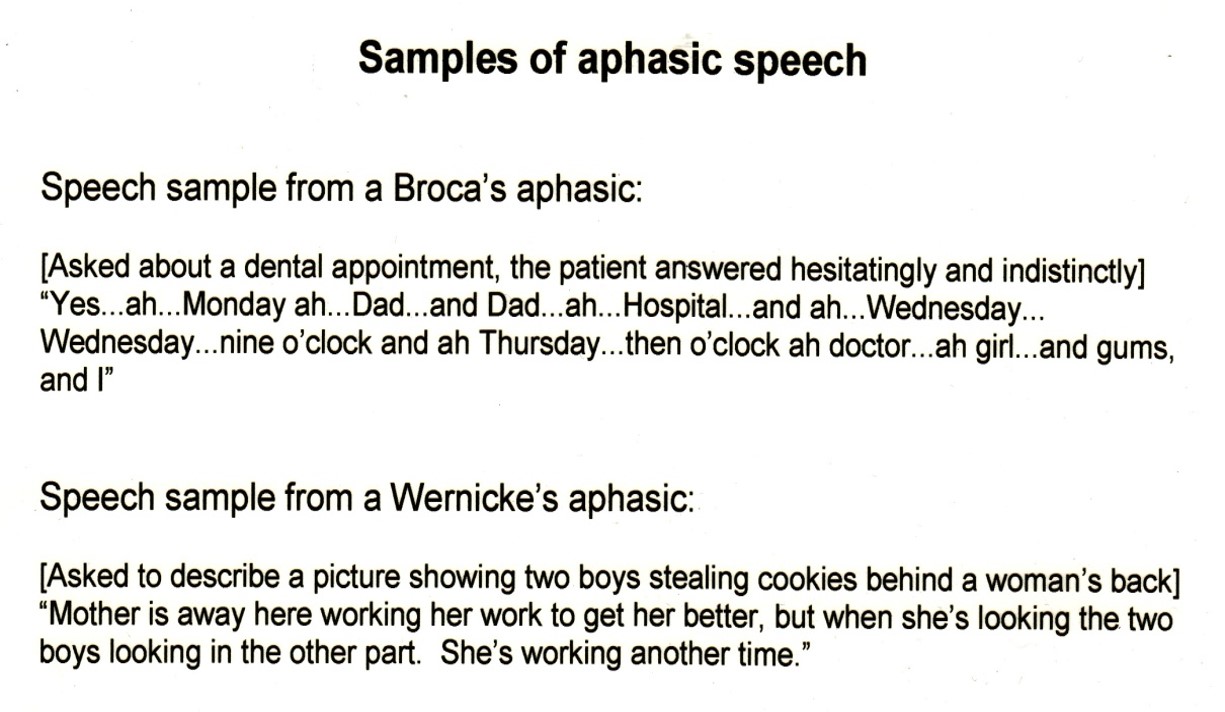
It's very hesitant, and it makes it hard to figure out exactly what he's saying, but you get the idea. This person is trying to convey that they went to a doctor's appointment that was for their teeth—therefore dentist—their father sent them or came with them, and it was probably in the morning. You look at Broca’s aphasic, you can get the point. But Wernicke’s aphasics are a different matter. In this scenario, we see a Wernicke’s aphasic. They have a picture in front of them with two boys stealing cookies behind a woman's back. Now, I realize both examples are very difficult to understand. But I think you would agree with me that, with the Broca’s aphasic, you got some of what this person was trying to convey; it was difficult, but you could do it. In the case of the Wernicke’s aphasic, it's impossible. Yes, the person says that there's a mother and that there's two boys. But there's nothing about a kitchen; there's nothing about cookies; there's nothing with stealing; there's nothing about anything. This is what makes Wernicke’s so difficult to treat is the processing part of it. In most cases Wernicke’s aphasics don't necessarily understand that they're not communicating; sometimes they do, but frequently they don't.
All that being said, what aphasia tells us and helps us to understand is that language is independent of intelligence. Even at his worst moments, my husband may not have always been able to communicate exactly what he wanted to say. But he was just as intelligent as he was before the stroke. Now he's able to communicate pretty well. It just goes to show that there's always hope.
Examples of Aphasia
All videos below are captioned.
Wernicke's Aphasia
Broca's Aphasia
Sarah Scott, 1 year out from her stroke:
Sarah Scott, 2 years out from her stroke:
Sarah Scott, 5 years out from her stroke:
Bilingual Aphasia
More on Aphasia
Watch this TedEd video in which Susan Wortman-Jutt explains a bit more about the affects of aphasia on the brain. (The video is captioned.)

