12.5: STI Prevention
- Page ID
- 167230
Stigma will not stop the spread of STIs. Testing, treatment and education will.

- Condoms and other barriers, used consistently and correctly, for genital, anal and oral contact can help prevent the spread of STIs.
- Talk to partners about testing, Know the status of your partners.
- Sufficient lubrication for vaginal and anal penetration can help prevent cuts and tears that can allow infections to get in. Be generous when using lube and be sure the lubricant is compatible with condoms if you are using them.
- For HIV prevention, PrEP, PEP and U=U are other powerful tools.
For more on this watch: Planned Parenthood on Getting Tested

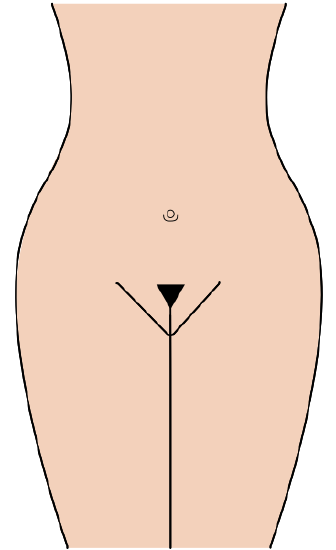
Public Hair: Consider Keeping it
Pubic hair provides some protection from STIs, especially those that are passed via skin-to-skin contact. With hair removal (shaving, waxing or tweezing) tiny wounds can be created that create a place for bacteria, parasites and viruses to enter. Also, the hair itself provides a protective layer against skin abrasions and injury that can come with friction during sexual activity. With hair removal, people sometimes end up with bumps and skin irritation they then mistake for an STI, so often it causes more stress than it’s worth. The only upside of pubic hair removal as far as STIs is that pubic lice are rarely seen these days as they have lost their bushy habitat.
Partner Notification
Notifying partners of a possible STI exposure is key in stopping transmission. Some public health departments will do anonymous partner notification as needed. This would usually be for HIV or syphilis. There are apps available to do anonymous notification. Partners should be treated as recommended by the CDC.
Expedited Partner Treament (EPT)
When someone tests positive for chlamydia and receives treatment, it is recommended that all partners be treated with antibiotics in order to prevent re-infection. Often, a medical provider can prescribe partner packs of antibiotics to a patient to give to their partner(s) as needed. This is known as expedited partner treatment. Unfortunately, this is not as easily done for gonorrhea and syphilis, since the preferred treatment for those infections includes an injection. In that case partners are advised to seek medical treatment at a clinic.

A Shameful Legacy of Racism in Medicine: The Tuskegee Study of Untreated Syphilis in the Negro Male
The Tuskegee experiment, first discussed in Chapter 2 serves as an important lesson on multiple fronts. In 1932, the Public Health Service (which later became the CDC) of the United States, along with the Tuskegee Institute, began a syphilis study in Macon County, Alabama. The participants included 600 Black men– 399 with syphilis and 201 without. The men were not told they had syphilis nor that the study had anything to do with syphilis. They were told they were being treated for “bad blood.” The study was based on the racist hypothesis that Black people had deficient cranial capacity and higher sex drive than whites. Even when penicillin was discovered to be highly effective treatment for syphilis in the mid-1940s, the researchers did not offer it to subjects, nor were subjects given the choice to quit the study. They were kept off draft lists for World War II, since syphilis testing was done when one entered the armed forces, and the researchers did not want the men to find out they had syphilis and receive treatment. The researchers had decided they wanted to study the progression of the disease without treatment. They made it clear the idea was to follow the men until death so they could study the cadavers for disease progression.

Originally, the study was projected to last 6 months, yet it went on for 40 years, finally ending in 1972, when it was leaked to the press what was happening. There were several whistleblowers inside the CDC who attempted to stop the study for many years before that date, but the CDC chose to continue. By 1972, 28 of the patients had died directly from syphilis, 100 had died from complications related to syphilis. Forty of the patient’s wives had syphilis and 19 of their children had been born with congenital syphilis. This study was an incredible violation of ethical standards. The harm done to the men and their families was egregious. It has also left a legacy of mistrust between the Black community and U.S. public health. It wasn’t until 1997 that the United States gave a formal apology to the few men who had been in the study who were still alive at that time and to their families. There is a Memorial Legacy Museum at Tuskegee University.

The Voices for Our Fathers Legacy Foundation, President Lillie Tyson Head, pictured above (daughter of Freddie Lee Tyson) was started by the families of the men to preserve the legacies and history of the 623 men victimized in the United States Public Health Service Syphilis Study, foster social justice, education and public health.
Talk to partners about testing. If you’ve tested, that can be a conversation starter. You can say “I just did my routine STI testing. When was the last time you tested?” I talk to people sometimes who say “well, he says he doesn’t need to test” or “she looks clean” or “I don’t think I have anything.”
The only way to know for sure is to test. If you test negative, it doesn’t mean your partner is necessarily negative for everything. It’s possible to have an STI and not give it to someone right away. Asking someone to test is not about accusing them of something. It’s about being mature and responsible for your health and the health of your partner(s).
Consider throat and rectal swabs for chlamydia and gonorrhea when testing. They are often only offered to gay men or men having sex with men, but we all have throats and anuses. So, if you’ve given oral sex, ask for a throat swab and if you’ve received anal, ask for a rectal swab. Often you can do them yourself in the restroom at the testing lab.
Avoid language such as someone being “clean” when referring to someone who doesn’t have an STI. This implies that someone with an STI is dirty. This adds to stigma which ultimately makes people less likely to talk about STIs and to test. Instead, one could use the phrase “STI-free” as it is accurate and nonjudgmental.
If you’re having symptoms or a partner has told you they have an STI, and you are going for testing, let the medical provider know your reason for testing. If you have symptoms or have been exposed, they will likely prescribe you medicine right away, even before testing. It is still important to test, but this way you are not waiting for results to come back to get treatment, if needed.
One of the most challenging situations in dealing with STI testing is when there has been infidelity (often referred to as cheating) in a relationship. I talk to people on both sides of this issue. There can be lots of emotions involved from guilt, to shame to anger, resentment and sadness. I affirm that no matter the circumstances, testing is a good idea, for all parties involved. Even if the person who went outside the relationship says they are sure they didn’t get anything, I suggest that testing can be a way to start to rebuild trust in the relationship, if that is the goal.
Routine testing often includes HIV (if the person is HIV negative), syphilis, chlamydia and gonorrhea. If you have questions about herpes, HPV or other STIs, talk to a medical provider.
Just about every STI can be passed easily with oral sex, except HIV. It is highly unlikely that HIV could be passed that way, but chlamydia, gonorrhea, syphilis, HPV and herpes can all be passed with oral sex. Most people don’t use barriers for oral sex, but barriers are an option. Harm reduction for oral sex on a penis includes ejaculating outside of the mouth, as this can minimize risk for some STIs.


